By Jim English
The human heart is an organ of remarkable precision and reliability. Every minute this small pear shaped organ beats 72 times to completely recycle approximately five quarts of blood throughout the body. In an average lifetime the heart will steadily pound out more than 2.5 billion beats, a number most of us remain blissfully ignorant of, until something interrupts this tireless muscle and its life-giving rhythm.
Any change in the regular beating rhythm of the heart is defined as arrhythmia. Arrhythmia can manifest when the heart beats very fast (tachycardia) or very slowly (bradycardia). Arrhythmia is the result of interference with the electrical pathways that produce the heart’s rhythmic muscular contractions. Arrhythmias are responsible for over 400,000 deaths each year and are the cause of death for more than two-thirds of heart disease victims, killing more males in the Western world than any other disease.1
Arrhythmia Types
Arrhythmias Originating in the Atria:
- Sinus arrhythmia: Cyclic changes in the heart rate during breathing
- Sinus tachycardia: The sinus node sends out electrical signals faster than usual, speeding up the heart rate.
- Sick sinus syndrome: The sinus node does not fire its signals properly, so that the heart rate slows down or the rate changes back and forth between a slow and fast rate.
- Premature supraventricular contractions or premature atrial contractions (PAC): A beat occurs early in the atria, causing the heart to beat before the next regular heartbeat.
- Supraventricular tachycardia (SVT), paroxysmal atrial tachycardia (PAT): A series of early beats in the atria speed up the heart rate (the number of times a heart beats per minute). In paroxysmal atrial tachycardia, repeated periods of very fast heart beats begin and end suddenly.
- Atrial flutter: Rapidly fired signals cause the muscles in the atria to contract quickly, leading to a very fast, steady heartbeat.
- Atrial fibrillation: Electrical signals in the atria are fired in a very fast and uncontrolled manner. Electrical signals arrive in the ventricles in a completely irregular fashion, so the heart beat is irregular.
- Wolff-Parkinson-White syndrome: Very fast heart rates that may develop as the electrical signal ricochets between the atria and ventricles.
Arrhythmias Originating in the Ventricles:
- Premature ventricular complexes (PVC): An electrical signal from the ventricles causes an early heart beat that generally goes unnoticed. The heart then seems to pause until the next beat of the ventricle occurs in a regular fashion.
- Ventricular tachycardia: The heart beats fast due to electrical signals arising from the ventricles (rather than from the atria).
- Ventricular fibrillation: Electrical signals in the ventricles are fired in a very fast and uncontrolled manner, causing the heart to quiver rather than contract and pump blood.
Heart disease is a primary cause of arrhythmias but many arrhythmias occur in people with no underlying heart disease. Other external factors known to cause arrhythmias include: stress, caffeine, tobacco, alcohol, diet pills, and cold medications.
Sudden Cardiac Death
Sudden cardiac death, resulting from untreated rapid ventricular fibrillation, is the leading cause of death in the United States, affecting about 400,000 people each year and claiming the lives of about 70% of them. Sudden cardiac death occurs most often in people who have had past heart attacks (myocardial infarction), but can also occur in young healthy individuals. When the heart muscle doesn’t get enough oxygen and blood to properly contract and keep pumping blood to the rest of the body, ischemia results. Ischemia is a lack of oxygen to the heart. Ischemia causes problems such as angina pectoris (chest pain), and can lead to cardiac arrest, a heart attack from a sustained ventricular arrhythmia.2
Sudden cardiac death also occurs in individuals with no anatomical or electrophysiologic evidence of heart disease. In these people, silent (asymptomatic) ischemia from coronary artery spasm triggered by ventricular fibrillation may be the cause of cardiac arrest. According to the investigators, even in the absence of early chest pain and fixed coronary artery disease, transient ischemia can be severe enough to cause life-threatening arrhythmias. Over-exercising and acute stress commonly brings on ischemia, as well as stimuli such as stimulant drugs, all of which can cause sudden cardiac death.3
Anti-ischemic therapy (including stress control) may protect a person with silent or asymptomatic ischemia against ventricular arrhythmia, but individuals with ventricular tachycardia usually require additional antiarrhythmic therapy. Individuals with underlying coronary artery disease may need some form of intervention.
Standard Treatment Protocols
Many arrhythmias require no treatment due to the ability of the heart to tolerate markedly abnormal rhythms. Serious arrhythmias are treated in different ways depending on what is causing them. The treatment modalities include both pharmaceutical and nonpharmacologic therapies.
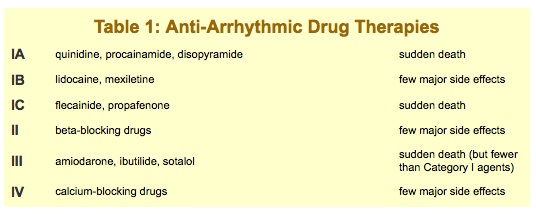
Antiarrhythmic drugs used to treat arrhythmia are often effective, but unfortunately, they are also expensive and have serious side effects. The majority of antiarrhythmic drugs have arrhythmogenic effects – in other words, they can cause arrhythmias themselves.4-6 In fact, controlled trials have shown that some anti-arrhythmia drugs actually increase the risk of death in some patients (see Table I, above). This has led to a wider application of nonpharmacologic therapies, including implantable defibrillators and radio-frequency catheter ablation that have become the dominant type of therapy for many patients with ventricular and supraventricular arrhythmias. But antiarrhythmic drugs may still play a role as an adjunctive therapy in certain patients and be used as first-line therapy in others.
Nutritional Alternatives to Anti-Arrhythmic Drugs
A number of natural agents have been shown to prevent the occurrence of arrhythmias while supporting normal heart rhythm and improving cardiac function. Other compounds have been shown to decrease the incidence and damaging effects of arrhythmias while improving myocardial functions. Some of these benefits include a positive inotropic effect (increased strength of heart contractions), increased myocardium (heart) tissue oxygenation, and scavenging of free radicals. These agents also help prevent cardiotoxicity of beta-blockers and certain psychotropic drugs. Working by different complementary mechanisms these natural compounds produce anti-arrhythmia actions and benefit cardiac functions without the side effects associated with some antiarrhythmic drugs.
Berberine
Berberine is the principal active ingredient in the herb goldenseal (Hydrastis Canadensis). Studies show that the alkaloid berberine is beneficial for ventricular arrhythmias due to lack of oxygen. Evidence also suggests that berberine administration can help prevent the onset of re-entrant ventricular tachyarrhythmias and sudden coronary death after myocardial ischemic damage.
Researchers studied the effects of berberine on individuals with ventricular tachyarrhythmias and found that 62% of patients had 50% or greater, and 38% of patients had 90% or greater, suppression of ventricular premature contractions.7 No severe side effects were observed from berberine therapy. In humans with refractory congestive heart failure, berberine produced several significant changes: a 48% decrease in systemic and a 41% decrease in pulmonary vascular resistance, along with a 28% decrease in right atrium and 32% decrease in left ventricular end-diastolic pressures.8 A measurable increase in cardiac index (45%), stroke index (45%), and left ventricular ejection fraction (56%) were also observed. There were increases in the indices of left ventricular performance and a decrease in arteriovenous oxygen uptake (28%) with no changes in total body oxygen uptake, arterial oxygen tension, or hemoglobin dissociation properties.
Coenzyme Q10
CoQ10 is highly concentrated in heart muscle cells due to the high-energy requirements of these cell types. Myocardial biopsies of patients with various cardiac diseases showed a CoQl0 deficiency in up to 75% of cases!9
Research has shown that orally administered CoQl0 can improve functioning of myocardial tissue, strengthening the heart’s contractions and making it beat more strongly (positive inotropic effect) and more regularly (anti-arrhythmia effect). CoQ10 also acts as an antioxidant to control free radicals produced during cardiac interventions (including angioplasty, thrombolysis, and surgery).
Accordingly CoQl0 has been used in the treatment of different heart disorders that include arrhythmias related to primary cardiomyopathies or secondary forms of heart failure.10 A 1998 study observed patients with acute myocardial infarction.11 For 28 days one group received 120 mg of CoQ10 and the other group received a placebo. After treatment, total arrhythmias were 9.5% in the CoQ10 group compared to 25.3% in the placebo group. CoQ10 produced a significant reduction in angina pectoris and left ventricular dysfunction. Non-fatal infarction and cardiac deaths also were significantly lower in the CoQ10 group. This shows that CoQ10 helps prevent potentially life-threatening dysrhythmias during the immediate period following a myocardial infarction. This is the period of time when arrhythmia has the greatest likelihood of causing death.
Taurine
Taurine is the most abundant free amino acid in the heart, surpassing the combined quantity of all other aminos. It modulates the activity of cAMP and affects enzymes in heart muscle that contribute to contractility. Taurine also plays a role in the metabolism of calcium and may affect entry of calcium into heart muscle cells where it is essential in the generation and transmission of nerve impulses.12 Research shows that taurine prevents arrhythmogenesis by limiting cardiac hypertrophy and calcium overload of the myocardium.13
Following ischemia or necrosis, taurine levels drop to as low as one-third of normal levels. Taurine protects the ischemic heart against reperfusion-induced arrhythmias, via both its properties as a membrane stabilizer and oxygen free radical scavenger.14
Arrhythmias characteristic of acute myocardial ischemia may be due to loss of intracellular taurine. Researchers found that intravenous administration of taurine prevented arrhythmias caused by digitalis. Taurine also inhibited the drop in potassium levels inside heart cells that can cause electrical instability and arrhythmias.15 Supplemental taurine has been shown to reduce the occurrence of myocardial infarction and lower elevated blood pressure by reducing sympathetic tone.16
Conclusion
Death resulting from disruptions within the electrical pathways that control heart rhythm contribute to over 400,000 deaths each year. While antiarrhythmic drugs are effective, they are also somewhat expensive and can have serious side effects, not the least of which is a tendency to initiate the very event being treated. A number of cost effective supplements have been shown to prevent the occurrence of arrhythmias, support normal heart rhythm, improve cardiac function and decrease the incidence and damaging effects of arrhythmias, without the serious side effects of prescription medications.
References
1. “Arrhythmias/Rhythm Disorders,” Fact sheet, National Heart, Lung and Blood Institute, NIH Publication No. 95-2264, September 1995.
2. Managing Ventricular Fibrillation in Patients with Silent Myocardial Ischemia Reprinted from Medical Sciences Bulletin 9/13/99, published by Pharmaceutical Information Associates, Ltd.
3. Heart Rate Variability and Ischemic Responses to Mental Stress: Results from the Psychophysiological Investigation of Myocardial Ischemia (PIMI) Study. Authors: D. Sheffield, et al. Ref: 48th annual meeting of the American College of Cardiology. March, 1999.
4. Podrid PJ, Lampert S, Graboys TB, Blatt CM, Lown B. Aggravation of arrhythmia by antiarrhythmic drugs – incidence and predictors. Am J Cardiol 1987;59:38E-44E.
5. Echt DS, Liebson PR, Mitchell LB, et al. Mortality and morbidity in patients receiving encainide, flecainide, or placebo – the Cardiac Arrhythmia Suppression Trial. N Engl J Med 1991;324:781-8.
6. Teo KK, Yusuf F, Furberg CD. Effects of prophylactic antiarrhythmic drug therapy in acute myocardial infarction: an overview of the results from randomized controlled trials. JAMA 1993;270:1589-95.
7. Huang W. Ventricular tachyarrhythmias treated with berberine. Chung Hua Hsin Hsueh Kuan Ping Tsa Chih 1990;18:155-156,190.
8. Marin-Neto JA, Maciel BC, Secches AL, Gallo Junior L. Cardiovascular effects of berberine in patients with severe congestive heart failure. Clin Cardiol 1988;11:253-260.
9. Folkers K., Vadhanavikit S., Mortensen S.A. (1985) Biochemical rationale and myocardial tissue data on the effective therapy of cardiomyopathy with coenzyme Q10. In: Proc. Natl. Acad. Sci., U.S.A., vol. 82(3), pp 901-904.
10. Mortensen S.A., Vadhanavikit S., Muratsu K., Folkers K. (1990) Coenzyme Q10: Clinical benefits with biochemical correlates suggesting a scientific breakthrough in the management of chronic heart failure. In: Int. J. Tissue React., Vol. 12 (3), pp 155-162.
11. Singh RB; Wander GS et al Randomized, double-blind placebo-controlled trial of coenzyme Q10 in patients with acute myocardial infarction. Cardiovasc Drugs Ther, 12(4):347-53 1998 Sep.
12. Sebring, L. A. and Huxtable, R. J. Cardiovascular actions of taurine. In: Sulfur Amino Acids: Biochemical & Clinical Aspects, 1983.
13. Hernandez, J.; Artillo, S.; Serrano, M. I.; and Serrano, J. S. Further evidence of the antiarrhythmic efficacy of taurine in the rat heart. Res. Commun. Chem. Patho. Pharma., 43(2):343-346, 1984.
14. Bousquet, P.; Feldman, J.; Bloch, R.; and Schwartz, J. The central cardiovascular effects of taurine. Eur. J. Pharmacol, 98:269-273, 1984.
15. Wessberg, P.; Hedner, T.; Hedner, J.; and Jonason, J. Effects of taurine and a taurine antagonist on some respiratory and cardiovascular parameters. Life Sci., 33:1649-1655, 1983.
16. Finley RJ; Inculet RI; et al: Major operative trauma increases peripheral amino acid release during the steady-state infusion of total parenteral nutrition in man. Surgery, 99(4):491-500 1986 Apr.












[…] https://nutritionreview.org/2013/04/drugfree-alternatives-arrhythmia/ Researchers studied the effects of berberine on individuals with ventricular tachyarrhythmias and […]
[…] https://nutritionreview.org/2013/04/drugfree-alternatives-arrhythmia/ Researchers studied the effects of berberine on individuals with ventricular tachyarrhythmias and […]