By Jim English
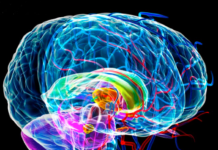
The human brain is the most elegant and complex structure ever devised. Comprising some ten billion neurons and supportive cells, no other organized structure – organic or silicon – can begin to match the sheer complexity and processing power of the human brain. It regulates virtually all life systems while simultaneously generating the thoughts, dreams and feelings that define us and shape our perception of reality.
Every thought, concept, opinion, belief and emotion arises from the untold millions of chemical and electrical reactions that occur in the brain every second. And to power all of this activity the brain places a huge demand on the body’s energy reserves. Though it accounts for a mere two percent of body’s weight, the brain greedily consumes more than twenty percent of the body’s available energy in the form of oxygen and glucose.
The Aging Brain
Time takes a terrible toll on the human brain. Many tissues, such as the skin and liver cells, have the capacity to regenerate, but this trait is not shared by brain cells – once a brain cell is lost, it is gone forever. By age seventy most people lose ten percent of their original brain cells to the effects of “normal” aging. This continual loss of brain cells is further aggravated by damage from other age-related conditions, such as hypertension, arteriosclerosis (hardening of the arteries), diabetes, and cerebrovascular diseases (CVD) such as cerebrovascular insufficiency, strokes and multi-infarct dementia (MID).
Dementia
Dementia is defined as the loss of cognitive or intellectual functions. Unlike occasional forgetfulness, dementia is marked by a profound impairment of memory as well as the loss of additional, complex abilities required for problem-solving, decision making, spatial orientation, and even the ability to put simple words together to communicate.
Dementia is a permanent, progressive disease that mostly affects the elderly, who, over time may lose the ability to function normally and require round-the-clock care. It is estimated that up to 8 percent of all people over 65 suffer from some form of dementia, and that the number of cases doubles with every additional five years, leading to the estimate that anywhere from 20 percent to 50 percent of people in their 80s suffer from dementia.
There are close to fifty different causes of dementia, including neurological disorders (Alzheimer’s disease), vascular disorders (multi-infarct disease), inherited disorders (Huntington’s disease), and infections (viruses such as HIV).
A common factor shared by all of these disorders is the reduction in the flow of blood and oxygen to the brain. Reduced blood flow, aside from starving brain cells of needed fuel, also increases the production of free radicals that further damage cell membranes and accelerate brain cell death. As the number of lost brain cells grows – from the ravages of age or the debilitating effects of degenerative diseases such as Alzheimer’s – mental deterioration continues. Memories begin to fade and the ability to form new thoughts and solve problems is further reduced. Depression, incontinence, disorientation, speech disturbances, tremor, muscle weakness, tinnitus (ringing in the ears), and loss of both visual acuity and coordination also increase as the conditions progress.
Alzheimer’s Disease
Alzheimer’s disease (also called “senile dementia of the Alzheimer type”) is a chronic and progressive degenerative neurological condition. Alzheimer’s currently afflicts over four million people in the United States, and accounts for up to 60 percent of all cases of dementia. Alzheimer’s commonly appears after age fifty, and from age sixty-five on, the risk of developing the disease doubles with every additional five years of age. As if these numbers weren’t bad enough, they are expected to almost double in the coming decades, placing a further drain on health care resources, and leaving almost no family untouched.
While there is currently no cure for Alzheimer’s disease, exciting new research shows that several nutrients may help to halt the destructive progression of dementia and improve cognitive function of patients suffering from Alzheimer’s and other forms of dementia.
Hope for Aging Brains
While medical researchers and pharmaceutical companies race to patent new (and profitable) treatments for Alzheimer’s and other degenerative brain conditions, a number of existing nutritional compounds have already been proven to safely support healthy brain function while protecting and prolonging cognitive ability. Supported by numerous double-blind controlled trials in Europe and the US, these supplements can slow down the age-related loss of higher-level cognitive functions that can appear in healthy individuals as young as fifty years of age.
Huperzine
Alzheimer’s is characterized by the destruction of nerve cells in key areas of the brain devoted to higher mental function. Most noticeable is the loss of presynaptic cholinergic neurons that results in a dramatic decrease in brain levels of acetylcholine, a neurotransmitter involved in memory and intracellular communication. Research has shown that levels of acetylcholine are deficient in the brains of patients with Alzheimer’s disease, and what little acetylcholine is produced is quickly broken down by the enzyme, acetylcholinesterase (AchE), contributing to the loss of memory and other cognitive functions.
Huperzine is a nutritional supplement that readily crosses the blood-brain barrier to prevent acetylcholinesterase (AchE) from destroying acetylcholine. By inhibiting AChE and increasing acetylcholine concentrations in the brain, Huperzine A has been shown to be effective in alleviating some of the symptoms associated with acetylcholine deficiencies.
Researchers have demonstrated that patients suffering from Alzheimer’s and various other memory disorders gain significant benefit from huperzine, both in terms of memory and life quality. In one study, researchers found that 58 percent of Alzheimer’s patients experience significant improvement in both cognitive and memory function when given 200 mg of Huperzine per day.
Huperzine’s memory-enhancing properties suggest that it may be an effective agent for improving memory and learning in healthy humans as well. These findings suggest that Huperzine not only protects from the effects of Alzheimer’s and senile memory deficits, but also provides a unique and exciting supplement for supporting memory in the healthy aging human as well.
Vinpocetine
Vinpocetine is a powerful memory-enhancing nutrient that facilitates cerebral metabolism by improving cerebral microcirculation, stepping up brain cell ATP production, and increasing utilization of glucose and oxygen. Vinpocetine also selectively increases blood flow to the brain, particularly to impaired areas, without affecting blood flow to the rest of the body.
Because of its selective effects on improving cerebral circulation, vinpocetine is often used for the treatment of cerebral circulatory disorders such as memory problems, acute stroke, aphasia (loss of the power of expression), apraxia (inability to coordinate movements), motor disorders, dizziness and other cerebrovestibular (inner-ear) problems, and headache.
In studies involving 882 patients with neurological disorders ranging from stroke to cerebral insufficiency, vinpocetine was found to confer significant improvements in 62 percent of the patients. In one of the studies, cerebral insufficiency patients were asked to memorize a list of ten words. Without vinpocetine the subjects were able to memorize an average of six words. After a month of treatment the average went up to ten words.
Reactive oxygen species (ROS) are believed to play a crucial role in the neuronal damage occurring in ischemic injury (stroke) and neurodegenerative disorders. In studies designed to examine the antioxidant effects of vinpocetine to prevent the formation of ROS and lipid peroxidation in brain synaptosomes, researchers found that vinpocetine significantly decreased oxidative stress and inhibited ROS formation up to 83 percent.
The researchers concluded that the antioxidant effects of vinpocetine contributed to reducing neuronal damage in pathological situations.
Pyroglutamate
Pyroglutamate (2-oxo-pyrrolidone carboxylic acid, or PCA) is an amino acid found in vegetables, fruits, dairy products, and meats. Pyroglutamate is also present in large amounts in the human brain, cerebrospinal fluid, and blood.
Pyroglutamate is known to have a number of remarkable cognitive-enhancing effects. After oral administration, pyroglutamate passes into the brain through the blood-brain barrier and stimulates cognitive functions. Pyroglutamate improves memory and learning in rats, and has anti-anxiety effects in rats.
Pyroglutamate has also been shown to be effective in alcohol-induced memory deficits in humans and, more recently, in people affected with multi-infarct dementia. In these patients, the administration of pyroglutamate brought about a significant increase of attention and an improvement on psychological tests investigating short-term retrieval, long-term retrieval, and long-term storage of memory. A statistically significant improvement was observed also in the consolidation of memory.
In human subjects, pyroglutamate was compared with placebo in a randomized double-blind trial for assessing its efficacy in treating memory deficits in 40 aged subjects. Twenty subjects were treated with pyroglutamate and 20 with placebo over a period of 60 days. Memory functions were evaluated at baseline and after 60 days of treatment by means of a test made up of six memory tasks. The results show that pyroglutamate is effective in improving verbal memory functions in subjects affected by age-related memory decline.
Choline
Choline is a precursor to acetylcholine, a cholinergic neurotransmitter that declines with advancing age. Individuals predisposed to Alzheimer’s disease and other dementias, infants and children, diabetics, and athletes (who often have reduced plasma-choline levels after training or competition) may be at increased risk of choline deficiency.
Choline has been shown to have considerable potential for preserving the integrity of neuronal structures and in preventing some of the alterations in the central nervous system during aging. Choline supplementation appears to prevent the age-induced decline of the dendritic network composed of neurons that fire impulses to the cells. Choline increases the number of dendritic spines in the cerebral cortex of old mice and improves the animals’ learning performance.
Under conditions of increased demand for acetylcholine production, excess choline availability becomes a limiting factor for acetylcholine synthesis. When this additional, exogenous choline supply is unavailable, cholinergic neurons are able to use free choline taken from a choline “reservoir” to continue the synthesis of acetylcholine.
This process, termed “autocannabalism,” can lead to a decrease in the quantity and quality of membrane in these cells. Indeed, cholinergic neurons’ ability to use this alternative source of choline appears to contribute to their vulnerability in Alzheimer’s disease.
Researchers believe defects in choline-metabolism may play a central role in the development of Alzheimer’s disease as defects in choline transport exist in the cells of Alzheimer’s victims. Defects in choline metabolism may also be influential in Down’s syndrome, normal aging, Huntington’s disease, amyotropic lateral sclerosis, the familial dysautonomias, and the post-polio syndrome.
DMAE
DMAE (dimethylaminoethanol) is a nutrient found abundantly in fish and in human brains. In the brain DMAE is converted into choline, the precursor to acetylcholine. Because acetylcholine conducts nerve impulses within the brain, the increased acetylcholine synthesis seen after DMAE supplementation may improve memory and learning skills, elevate mood, prevent memory loss in elderly adults, and increase physical energy.
Studies suggest DMAE may work by inhibiting choline metabolism in peripheral tissues, causing free choline to accumulate in the blood, enter the brain and stimulate choline receptors. As the immediate precursor to choline, DMAE assists in the building and repair of cell membranes, particularly in the brain and central nervous system.
Animal studies have demonstrated that DMAE stimulates brain neurons and improves working memory performance. In one study, rats treated with DMAE demonstrated significant improvements in remembering how to negotiate a maze. In another study, mice trained to negotiate a maze demonstrated improved memory retention when treated with DMAE.
DMAE’s ability to stimulate acetylcholine synthesis has led researchers to explore its effects in senile dementia and Alzheimer’s. In a promising study, 14 senile dementia patients were treated with DMAE for four weeks. The dosage was gradually increased to 600 mg, three times daily, during the first two weeks, with no adverse effects. Although the patients experienced no improvement in cognitive function or memory, ten of the 14 patients experienced reduced depression, irritability and anxiety and increased motivation and initiative.
Phenylalanine
Phenylalanine is an essential amino acid and vital precursor used by the brain to produce dopamine, epinephrine and norepinephrine, stimulatory neurotransmitters that regulate mood, sex drive, memory, alertness, and learning. L-phenylalanine is also converted, via a separate pathway, into phenylethylamine (PEA), a mood-elevating compound that occurs naturally in the brain.
Phenylalanine has been found useful for alleviating depression. In one study forty depressed patients were treated with L-phenylalanine daily for up to six months. Doses started at 500 milligrams and gradually built up to between 3 to 4 grams daily. Patients also took 100 to 200 milligrams of vitamin B6 daily to enhance neurotransmitter synthesis.
Thirty-one patients (77 percent) reported positive benefits, and ten patients (25 percent) reported complete relief from symptoms of depression. The principal investigators reported that those who responded positively did so almost immediately.
Ginkgo Biloba
A number of clinical studies have shown that Ginkgo biloba can protect brain cells from damage caused by free radicals while improving blood circulation and oxygen delivery, particularly through the microcapillaries. In one study, researchers measured a fifty-seven percent increase in blood flow through capillaries within sixty minutes of giving Ginkgo to volunteers.
A second study by German scientists involved 60 patients diagnosed with cerebral insufficiency and depression. Patients receiving Ginkgo extract began to show marked improvement after only two weeks, with a significant reduction of many of their symptoms.
In another clinical trial of 166 patients over the age of sixty, researchers found that patients suffering from cerebral insufficiency showed a significant improvement following three months of treatment, confirming the efficacy of Ginkgo extract in cerebral disorders due to aging.
Researchers have also found that Ginkgo can be especially helpful when given to Alzheimer’s patients at the first sign of symptoms. In one published study, German scientists gave a daily dose of 120 mg of Ginkgo to twenty elderly patients exhibiting various early symptoms of dementia. The results were dramatic, and the patients receiving Ginkgo showed impressive improvements on a variety of clinical tests, as compared to patients receiving a placebo.
In one large study published in 1996, German researchers tested Ginkgo extract on a group of 222 patients, aged fifty-five or older, who were diagnosed with mild to moderate dementia caused by either Alzheimer’s disease or multi-infarct dementia. Patients were given either 240 milligrams of Ginkgo biloba extract, twice a day before meals, or a placebo, for the duration of the six-month long trial.
At the conclusion of the study the researchers reported that patients receiving Ginkgo showed a remarkable overall improvement in their condition, including a 300 percent increase in memory and attention as compared to those receiving the placebo pills.
The researchers concluded their report by stating that, in cases of dementia, Ginkgo extract could improve a patient’s quality of life while preserving independence and postponing the need (and expense) of full-time care.
Ginkgo Biloba and Multi-Infarct Dementia
The second most common cause of dementia in older people is multi-infarct dementia (MID), a condition that accounts for about fifteen percent of all cases of dementia. Multi-infarct dementia usually affects people between the ages of 60 and 75, and men are more likely to have multi-infarct dementia than women. MID is typically caused by a series of mini-strokes, also referred to as transient ischemic attacks (TIAs), that can occur when an artery in the brain either becomes blocked or ruptures. Strokes are generally caused by high blood pressure, high blood cholesterol, diabetes, and heart disease. Of these causes, the most important risk factor for multi-infarct dementia is untreated high blood pressure. In fact, it is extremely rare for a person to develop multi-infarct dementia without also having high blood pressure.
While these mini-strokes may or may not be noticed at the time, the effect on the brain is the same – brain cells become damaged by a lack of oxygen and die. Over time a series of mini-strokes can begin to destroy substantial portions of the brain that control speech and visual processing.
As with Alzheimer’s disease, Ginkgo has been shown to help patients suffering from MID by enhancing memory, alertness and overall quality of life. Additionally, given the underlying disorders that cause blood vessels to rupture, Ginkgo can also benefit patients suffering from MID by restoring elasticity and strength to stiff, weakened blood vessels.
Summary
Baby boomers and aging adults face a loss of cognitive powers and impaired mental functions. Research supports the role of a number of potent anti-aging therapies to slow brain aging and preserve cognitive function. Rather than waiting for signs of an irreversible decline in mental abilities or other, more serious cognitive problems, it would be prudent to take steps to support the brain’s ability to heal and self-repair. In short, we can take steps now to slow age-dependent brain cell changes, preserve vital functions, and maintain mental health and vigor.
References
1 Alzheimer’s Association, General Statistics and Demographics, www.alz.org/hc/overview/stats.htm.
2. Watkins PB, Zimmerman HJ, Knapp MJ. Hepatotoxic effects of tacrine administration in patients with Alzheimer’s disease. JAMA 1994 Apr 6; 271:992-8
3. Raves ML, Harel M, Pang YP, Silman I, Kozikowski AP, Sussman JL. Structure of acetylcholinesterase complexed with the nootropic alkaloid, (-)-huperzine A. Nat Struct Biol 1997 Jan;4(1):57-63.)
4. Xu SS; Gao ZX; Weng Z; Du ZM; Xu WA; Yang JS; Zhang ML; Tong ZH; Fang YS;Chai XS; et al, Efficacy of tablet huperzine-A on memory’ cognition’ and behavior in Alzheimer’s disease. Chung Kuo Yao Li, Hsueh Pao16:391-5, 1995.)
5. Santos MS, Duarte AI, Moreira PI, Oliveira CR Synaptosomal response to oxidative stress: effect of vinpocetine. Free Radic Res 2000 Jan;32(1):57-66
6. Haubrich DR, Gerber NH, Pflueger AB. Deanol affects choline metabolism in peripheral tissues of mice. J Neurochem. 1981; 37(2):476-82.
7. Dean W, Morgenthaler J. Smart Drugs & Nutrients.
8. Kostopoulos GK, Phillis JW. The effects of dimethylaminoethanol (deanol) on cerebral cortical neurons. Psychopharmacol Commun. 1975; 1(3):339-47.
9. Levin ED, Rose JE, Abood L. Effects of nicotinic dimethylaminoethyl esters on working memory performance of rats in the radial-arm maze. Pharmacol Biochem Behav. 1995; 51(2-3):369-73.
10. Flood JF, Smith GE, Cherkin A. Memory retention: potentiation of cholinergic drug combinations in mice. Neurobiol Aging. 1983; 4(1):37-43.
11. Nagy I, Nagy K. On the role of cross-linking of cellular proteins in aging. Mech Ageing Dev. 1980;14(1-2):245-51.
12. Marsh GR, Linnoila M. The effects of deanol on cognitive performance and electrophysiology in elderly humans. Psychopharmacology (Berl). 1979; 66(1):99-104.
13. Ferris SH, Sathananthan G, Gershon S, Clark C. Senile dementia: treatment with deanol. J Am Geriatr Soc. 1977; 25(6):241-4.
14. Fisman M, Mersky H, Helmes E. Double-blind trial of 2-dimethylaminoethanol in Alzheimer’s disease. Am J Psychiatry. 1981; 138(7):970-2.
15. Lewis JA, Young R. Deanol and methylphenidate in minimal brain dysfunction. Clin Pharmacol Ther. 1975; 17(5):534-40.
16. Pfeiffer C. Nutrition and Mental Illness: An Orthomolecular Approach to Balancing Body Chemistry. Healing Arts Press.
17. Rimland B. Controversies in the treatment of autistic children: vitamin and drug therapy. J Child Neurol. 1988; 3 Suppl:S68-72.
18. Cenni, A., et al. “Pharmacological Properties of a Nootropic Agent of Endogenous Origin: D-Pyroglutamic Acid.” Journal of Drug Development. 1988, 1, pp. 157-62.
19. Drago, F., Continella, G., Valerio, C., D’Agata, V., Astuto, C., Spardaro, F., Scapagnini, U. “Effects of Pyroglutamic Acid on Learning and Memory Processes of the Rat.” Acta Therapeutica. 1987, Vol. 13, pp. 587-94.
20. Filippo, V., Spignoli, G., Isidori, A. “Effects of Arginine Pyroglutamate on Growth Hormone in Children.” Clinical Trials Journal. 1987, Vol. 24, pp. 387-90.
21. Grioli, S. et al. “Pyroglutamic Acid Improves the Age Associated Memory Impairment.” Fundamental and Clinical Pharmacology. 1990, Vol. 4, pp. 169-73.
22. Moret, C., Briley, M. “The Forgotten Amino Acid Pyroglutamate.” Trends in Pharmacological Sciences. 1988, Vol. 9, pp. 278-9.
23. Paoli, F., Spignoli, G., Pepeu, G. “Oxiracetam and D-Pyroglutamic Acid Antagonize a Disruption of Passive Avoidance Behavior Induced by the N-Methyl-Aspartate Receptor Antagonist 2-amino-5-phosphonovalerate.” Psychopharmacology. 1990, 100, pp. 130-1.
24. Spignoli, G., Magnani, M. Pepeu, G. “Pyroglutamic Acid Antagonizes the Amnesic Effect and the Decrease in Brain Acetylcholine Level Induced by Scopolamine.” Pharmacological Research Communications. 1987, Vol. 10, pp. 901-7.
25. Sabelli HC. Clinical studies on the phenylethylamine hypothesis of affective disorder: urine and blood phenylacetic acid and phenylalanine dietary supplements. J Clin Psychiatry 1986;47:66-70.
26. Fischer E et al. Therapy of depression by phenylalanine. Arzneimittelforsch 1975;25:132.
27. Heller B et al. Therapeutic action of D-phenylalanine in Parkinson’s disease. Arzneimittelforsch 1976;26:577-579.
28. Budd K. Use of D-phenylalanine, an enkephalinase inhibitor, in the treatment of intractable pain. Adv Pain Res Ther 1983;5:305-308.
29. Rai, GS, et al. A double-blind, placebo-controlled study of Ginkgo biloba extract (“Tanakan”) in elderly outpatients with mild to moderate memory impairment. Current Medical Research and Opinion, 1991; 12:350-355.
30. Rapin, JR, et al. Local cerebral glucose consumption. Effects of Ginkgo biloba extract. Presse-Medicale, 1986; 15:1494-1497.
31. Taillandier, J, et al. Ginkgo biloba extract in the treatment of cerebral disorders due to ageing. Presse-Medicale, 1986; 15:1583-1587.
32. Vesper, J, Hansgen, K-D. Efficacy of Ginkgo biloba in 90 outpatients with cerebral insufficiency caused by old age. Results of a placebo-controlled double-blind trial. Phytomedicine, 1994; 1:9-16.
33. Vorberg, G. Ginkgo biloba extract (GBE): a long-term study of chronic cerebral insufficiency in geriatric patients. Clinical Trials Journal, 1985; 22:149-157.
34. Oberpichler, H, et al. Effects of Ginkgo biloba constituents related to protection against brain damage caused by hypoxia. Pharmacological Research and Communications, 1988; 20:349-368.












[…] Memory Enhancement and Cognitive Function – While there is currently no cure for Alzheimer’s disease, exciting new research shows that several nutrients may help to halt the destructive progression of dementia and improve cognitive function … C. Senile dementia: treatment with deanol. […]
[…] Memory Enhancement and Cognitive Function – Nutrition Review […]