By Jim English
Allergies arise from an imbalance in the immune system that causes the body to overreact to normally harmless irritants (allergens). This abnormal process triggers an inflammatory response that leads to tissue swelling, redness, heat and pain, accompanied by exudation of fluids. In upper respiratory allergies, the eyes, sinuses, nose, throat and upper lung tissues are all affected to varying degrees. Left untreated, these symptoms can result in chronic swelling of the sinuses and increased risk of infection.
The best treatment for allergies is to simply avoid substances that trigger a reaction. Since this is not always possible, many allergy sufferers turn to prescription and over-the-counter medications for relief. While antihistamines and other drugs may offer some help, they can also cause serious problems. Typical antihistamines can make even the simplest of tasks, such as driving a car or operating heavy machinery, difficult, or even dangerous. More importantly, simply blocking histamine doesn’t address the underlying imbalance, and over time allergy symptoms can become more severe and difficult to treat.
Traditional Chinese medicine has enjoyed great success in developing highly effective herbal formulas for rapid relief from seasonal and perennial allergy miseries. These proprietary blends of essence herbs quickly and safely relieve common allergic symptoms caused by:
- Pollen
- House dust
- Dust mite particles
- Mold spores
- Pet dander
- Chemical pollutants
Understanding how the right combination of herbs can work to 1) gently interrupt the allergic response, 2) reduce inflammation and 3) aid in resolving the underlying imbalance requires a brief review of the three stages of the allergic response: sensitization, acute inflammation, and chronic tissue damage.
Stage 1: Sensitization to Allergens
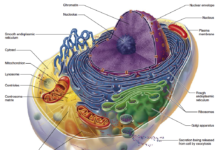
In Stage 1, for reasons not yet fully understood, the immune system mistakenly identifies an otherwise harmless substance as a potential threat to the body. While there are no allergic symptoms at this stage, the immune system is already hard at work preparing for battle with the newly targeted allergen.
The process starts as a specialized class of cells called macrophages attach themselves to the targeted allergen. After destroying the substance, the macrophages pass fragments of the allergen on to a class of cells called T-lymphocytes (T-cells). T-cells respond by secreting acytokine, called interleukin-4, that triggers another class of lymphocytes, B-lymphocytes, to begin producing immunoglobulin E (IgE) antibodies specific to that allergen.
Individuals prone to allergies are known to create abnormally high levels of IgE antibodies, making them susceptible to allergic rhinitis, asthma, atopic dermatitis and anaphylactic reactions.
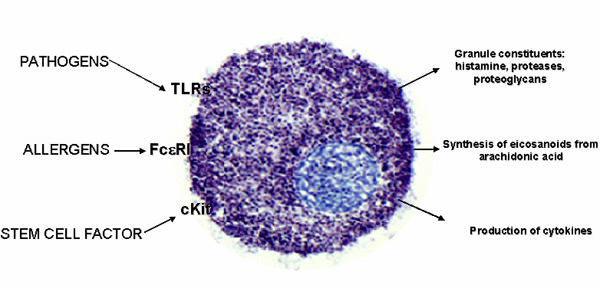 |
As IgE antibodies circulate through the blood, they attach to receptors on mast cells located in connective tissues. Mast cells are especially concentrated in small blood vessels and epithelial tissues covering the skin and lining the respiratory and digestive tracts (Fig. 1). In addition to mast cells, IgE antibodies also attach to basophils, a specialized type of white blood cell that can exit small blood vessels to congregate around allergens. Once this first stage is complete, a future exposure will cause the targeted allergen to bind to the newly created IgE molecules residing on the surfaces of mast cells and basophils, leading to Stage Two, acute inflammation.
Stage 2: The Chemical Cascade Begins
Stage 2 begins when the prepared immune system encounters the allergen at a future date. This time the immune system goes into action as the IgE antibodies bind to the allergen. This results in the activation of a chemical cascade as mast cells begin to “degranulate” and release histamine and other inflammatory chemicals – cytokines, interleukins, leukotrienes, andprostaglandins – into the surrounding tissues.
Histamine
Histamine dilates blood vessels, causing localized redness and swelling due to the release of fluids. Histamine also constricts bronchial tubes, impairs breathing, stimulates production of mucus in the respiratory system, and irritates nerve endings, causing itching and pain. Histamine is responsible for many common allergic symptoms, such as sneezing, itching, sinus congestion, wheezing, coughing, shortness of breath, and skin swelling, hives or rashes.
Leukotrienes
In addition to directly contributing to inflammation, histamine also initiates the release of leukotrienes (leukotrienes B4, C4, D4 and E4). These leukotrienes, especially leukotriene D4, are ten times more potent than histamine. In addition to constricting bronchial muscles, leukotrienes also act on blood vessels, causing them to become leaky and resulting in skin eruptions and swelling.
Prostaglandins
Unlike histamine, which is produced in both mast cells and basophils, prostaglandins are only released by the mast cells. One prostaglandin in particular, D2 (PGD2), is an even more potent bronchoconstrictor than histamine, though less so than the leukotrienes. Elevated PGD2 levels have been measured in secretions aspirated from the lungs of asthmatics and in nasal secretions from patients with nasal allergies.
Stage 3: Prolonged Immune Activation
Stage 3, or the “late phase” response is characterized by prolonged immune activation, usually occurring 2 to 24 hours after the initial allergic response. This late phase is characterized by the influx of additional inflammatory cells, as mast cells and neighboring tissues synthesize additional molecules that induce circulating basophils, eosinophils, and other cells to migrate into affected tissues. This generates a new wave of symptoms as the newly recruited cells begin secreting chemicals of their own to sustain the inflammatory process, resulting in local tissue damage. These late-phase inflammatory chemicals include additional immune mediators – leukotrienes, prostaglandins, thromboxanes, and platelet activating factors – that further aggravate the progression towards a state of chronic inflammation.
Cytokines
Several cytokines have been shown to play an important role in the regulation of IgE synthesis and the accumulation of eosinophils – white blood cells responsible for combating infection and parasites – during allergic reactions. One cytokine, interleukin 4 (IL-4), has been proven to be essential for promoting the production of IgE antibodies. Another cytokine, interleukin 5 (IL-5), also plays a key role in the maturation, activation and survival of eosinophils (increased numbers of eosinophils in blood and tissues is a characteristic feature of allergic disease).Tumor necrosis factor alpha (TNF alpha) is another cytokine that is produced rapidly during an allergic reaction. TNF-alpha regulates the secretion of additional cytokines to further attract and activate eosinophils while promoting the accumulation of inflammatory cells at the onset of the allergic reaction.
How Herbs Aid in Inhibiting Allergic Reactions
Symptoms of allergy are highly varied, because different allergens stimulate the immune system at different sites in the body. Despite this diversity, the goals of anti-allergic treatment are similar: to interrupt the instigation of inflammation (stage 2); to resolve chronic tissue damage (stage 3); and to desensitize the immune system so that it does not overreact to allergens in the first place (stage 1). Advanced herbal formulas can provide quick-acting symptomatic relief for upper and lower respiratory allergies while strengthening the immune system to shorten the allergy season.
One advanced formula combines ten traditional Chinese herbs that have been specifically selected for their ability to quickly and safely relieve allergic symptoms while gently resolving the underlying imbalance that triggers allergic disorders (see chart above). Many of these herbs have been shown to disrupt the chemical pathways that promote local tissue inflammation. While these herbs reduce acute attacks on local tissues, others assist in reducing swelling while clearing out fluid exudates generated by chronic inflammation.
These herbs are further supported by specialized herbs shown to aid the immune system by desensitizing it to prevent future allergic reactions. Centipeda, Xanthium and Angelica are well-known for their abilities to clear nasal and sinus congestion. Centipeda and Schizonepeta also aid in reducing the inflammation responsible for itching of the eyes and respiratory tissues.Fritillaria, Angelica, Paeonia and Platycodon have been shown to reduce tissue swelling, another source of allergy miseries. And finally, the combination of Centipeda, Fritillaria, Platycodon and Licorice are traditionally used to reduce the accumulation of exuded fluids.
Rapid Relief From “Brain Fog”
Brain fog is a term used to describe some of the most disabling allergy symptoms, including loss of concentration, impaired memory, irritability, fatigue, exhaustion and poor sleep. Caused by the inflammatory effects of histamine on brain tissues, brain fog severely impairs mental function, contributes to depression and degrades quality of life of people dealing with chronic allergic reactions.
Gastrodia is largely responsible for relieving brain fog. Modern research suggests that gastrodia aids in improving memory by promoting blood flow to the brain. Gastrodia also enhances the ability of other herbs to quickly reach inflamed brain tissues to reduce inflammation, control pain and reduce mental confusion.
The other traditional use for Gastrodia is to resolve neurasthenia – nervous exhaustion characterized by a sense of weakness or fatigue, easy exhaustion on the slightest effort, headache, sensitivity to light, inability to concentrate, irritability and complaints of poor memory, poor sleep, numerous constant, varying aches and pains. Along with depression, these are all common complaints for people with severe and chronic allergic reactions. They are also the most disabling in terms of quality of life – the ability to play, work, and live a full life. Neurasthenia is thought to involve vasomotor disturbances that affect the nerves having control of the blood vessels. Gastrodia is one of the most commonly studied herbs in China for treating hypertension and for improving blood flow in the arteries of the brain.
Long-Term Benefits
Finally, two additional herbs provide a corrective effect on the immune system that accounts for the long-term benefits. Paeonia and Pseudostellaria promote liver and lung function respectively, to support proper immune function. With many of the allergy formula herbs directed to dampening the immune response to allergens, it is important to also support general immune system function. These herbs are likely, along with Gastrodia, to be partly responsible for helping to desensitize allergy sufferers to their various allergens.
Safety
In addition to a long history of use in Traditional Chinese Medicine for relieving allergic symptoms, traditional allergy support herbs have been studied and extensively analyzed for safety, allowing for a non-drowsy formula that doesn’t cause fatigue, fuzzy thinking or pose a danger when driving, as do most antihistamines. And since traditional allergy support herbs are not CNS stimulants, such as pseudoephedrine, users note that using the formula does not cause the “wired” sensation typical of certain OTC preparations.
Summary
Advanced allergy support herbal formulas combine the 5,000-year-old Eastern healing tradition with state-of-the-art manufacturing and pharmaceutical-quality processing to manifest the legendary rejuvenating powers of these healing agents. By exerting a gentle corrective effect to balance the immune system and dampen the tendency to overreact to allergens, the result is a simple, natural, and comprehensive solution for immediate relief from allergic symptoms while generating long-lasting benefit by resolving underlying imbalances that cause allergic reactions in the first place.
References
1. Wen W., China: A new medicine born of tradition. UNESCO Cour. 1979 Jul;7:25-7. PMID: 12309932.
2. Wang SP, Liu XM, Shang WF, Song J, Yu SR, Sun SM. Effect of Gastrodia on rotation induced motion sickness in mice. Space Med Med Eng (Beijing). 1999 Oct;12(5):342-5. PMID: 12022178.
3. Hayashi J, Sekine T, Deguchi S, et.al. Phenolic compounds from Gastrodia rhizome and relaxant effects of related compounds on isolated smooth muscle preparation. Phytochemistry. 2002 Mar;59(5):513-9. PMID: 11853746
4. Hsieh CL, Chiang SY, Cheng KS, et.al. Anticonvulsive and free radical scavenging activities of Gastrodia elata Bl. in kainic acid-treated rats. Am J Chin Med. 2001;29(2):331-41. PMID: 11527075.












Hi,
I came across the above write up and wanted to know that where can I access the above mentioned TCM treatment ,I am currently based in Mumbai, India and have high levels of IGE this getting bad allergic reactions.
It will be great if you can guide me to where I can access the above treatment.
Thanks
Abhisshek