by Jim English
Arthritis is a generic term for more than 100 different disorders, including osteoarthritis, rheumatoid arthritis, gout and fibromyalgia. Osteoarthritis, or wear-and-tear arthritis, is the most prevalent and disabling of all chronic conditions, affecting approximately 80 percent of all U.S. adults over 65. Osteoarthritis is a degenerative joint disease involving the loss of articular cartilage, the smooth, slippery tissue that covers the ends of bones that allows them to slide smoothly across each other as joints bend and flex.
Osteoarthritis can be caused by a variety of conditions (diabetes) or as a result of age-related thinning of cartilage. Obesity, which exerts mechanical stress on knee joints, is a recognized risk factor for osteoarthritis. Additionally, physical trauma, surgery, sports and occupational injuries are important factors for developing secondary osteoarthritis.
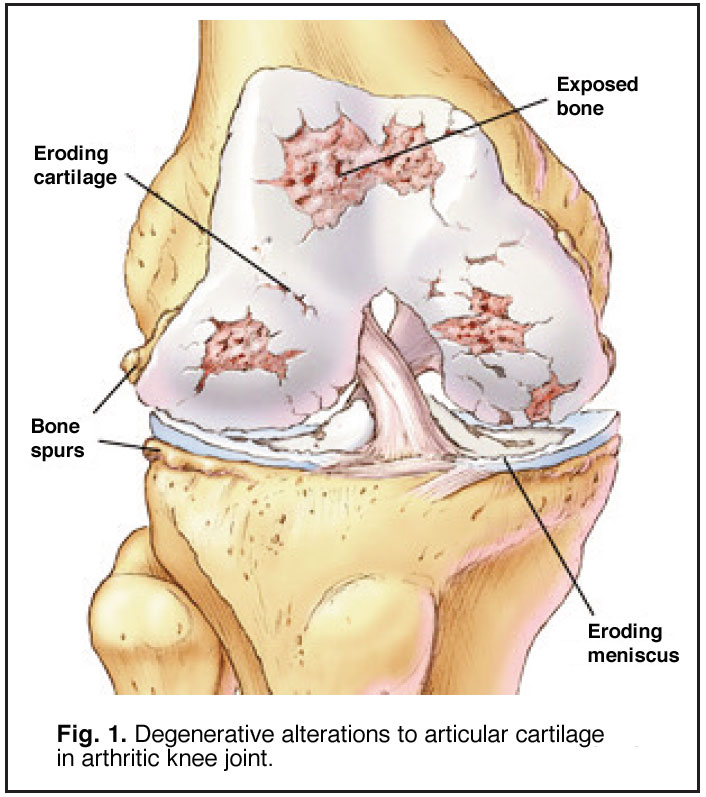 Osteoarthritis begins as a normal inflammatory response intended to protect joint tissues. For reasons not fully understood, the process goes awry, leading to degenerative changes in articular cartilage that cause the tissues to soften and swell up, making the cartilage less resistant to compressive forces and more susceptible to normal stresses (Fig. 1). Continued use of the joint further inflames the surrounding synovial membranes and irritates the cartilage, leaving the once-smooth surface covered with pits and crevasses that further compromise the affected joint. Eventually, articular cartilage can be completely stripped from the bones, necessitating joint fusion or surgical replacement with artificial joints.
Osteoarthritis begins as a normal inflammatory response intended to protect joint tissues. For reasons not fully understood, the process goes awry, leading to degenerative changes in articular cartilage that cause the tissues to soften and swell up, making the cartilage less resistant to compressive forces and more susceptible to normal stresses (Fig. 1). Continued use of the joint further inflames the surrounding synovial membranes and irritates the cartilage, leaving the once-smooth surface covered with pits and crevasses that further compromise the affected joint. Eventually, articular cartilage can be completely stripped from the bones, necessitating joint fusion or surgical replacement with artificial joints.
Treatment Options for Arthritis
There is currently no cure for arthritis and conventional medicine has little to offer beyond exercise (to increase joint flexibility), weight control (to reduce physical stress on the knees), and over-the-counter (OTC) or prescription anti-inflammatory and painkiller drugs to aid in managing arthritic symptoms.
• NSAIDs: Non-steroidal anti-inflammatory drugs (NSAIDs) continue to be the primary treatment options for arthritic inflammation and pain. Unfortunately, popular over-the-counter NSAIDs such as aspirin, ibuprofen and naproxen, can cause stomach ulcers, GI bleeding and perforations when taken for extended periods. Additionally, NSAIDs block the synthesis of new collagen matrix, the body’s main cartilage repair mechanism. By inhibiting this natural regenerative process, NSAIDs can temporarily dull pain and allow users to use their damaged joints completely unaware that they are actually speeding up the destruction of joint cartilage. In time, continuing joint damage exceeds the ability of NSAIDs to control pain, leading the patient to seek out more powerful analgesic agents.
• COX-2 Inhibitors: The introduction of a new class of NSAIDs known as COX-2 inhibitors was initially hailed as a breakthrough in arthritic pain treatment due to their analgesic properties and a general lack of gastrointestinal side effects. COX- 2 inhibitors work by reducing prostaglandins (chemical messengers) that cause pain and swelling. Unfortunately, COX-2 inhibitors also tend to increase risks of heart attacks and stroke by suppressing blood vessel dilation (vasodilation) and promoting formation of dangerous blood clots (thromboses).
Seeking Safer Options
Because of the risks associated with prescription and over-the-counter NSAIDs, use of alternative therapies, such as acupuncture, nutritional supplements and medicinal herbs, has risen sharply. Those seeking nutritional support for arthritis now have a wide range of choices, including natural compounds such as glucosamine, chondroitin sulfate, MSM and SAMe. Still, many find that success is often a hit or miss affair, requiring both luck and trial and error to determine which combination of supplements is most effective. Additionally, some supplements may be contraindicated due to interactions with pharmaceutical medications (i.e., warfarin, antidepressant drugs) and degenerative diseases such as diabetes and heart disease.
These concerns about side effects associated with conventional arthritis therapies have sparked a renewed scientific interest in traditional natural arthritis remedies. A current review of leading Chinese and English language medical journals reveals a surprising number of recently published studies detailing new insights into the biological and biochemical mechanisms of Chinese herbs that have historically been used to safely relieve arthritic inflammation, pain and swelling.
Herbs for Chronic Arthritic Pains
Chronic pain is one of the most difficult problems for those coping with arthritis. According to the CDC, arthritic pain is the nation’s leading cause of chronic disability, and nearly 19 million U.S. adults report that arthritic pain severely limits their daily activities.
While never pleasant, not all pain is bad. Short-term, acute pain serves as the body’s alarm system, warning us of danger (minor cuts, insect bites, etc.) while enabling us to learn from potentially damaging experiences. By contrast, the long-term pain associated with arthritis is a fixed, constant presence that is almost impossible to control.
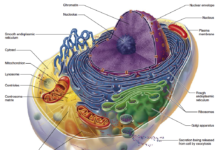
Arthritic pain begins when specialized receptors (nociceptors) are activated following damage to joint tissues. This activation results in the release of pro-inflammatory prostaglandins and cytokines (chemical messengers) such as IL-1 and TNF-alpha. These chemicals stimulate the release of additional inflammatory enzymes that further damage cartilage while blocking the body’s efforts to initiate repairs. As inflammation worsens, joint tissues swell and begin to compress pain nerves, resulting in degenerative nerve damage that triggers the release of even more inflammatory cytokines directly into the nerve roots. Over time this process alters the very structure of pain cells, causing them to become sensitized to the constant stimulus (Fig. 2).
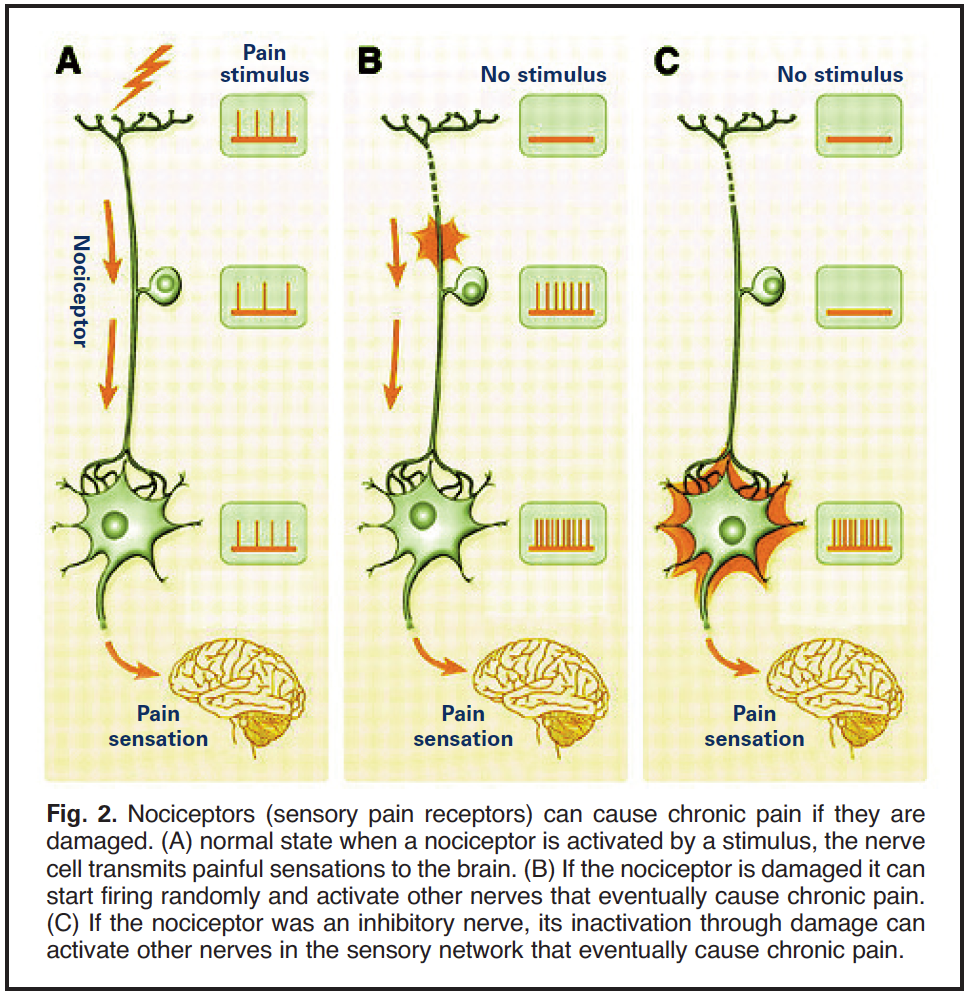 This process results in a lowering of pain threshold that directly amplifies pain signals while increasing sensitivity to pressure and temperature. In other words, the pain persists even after the original painful stimulus is no longer present.
This process results in a lowering of pain threshold that directly amplifies pain signals while increasing sensitivity to pressure and temperature. In other words, the pain persists even after the original painful stimulus is no longer present.
Inflammation-induced pain responds poorly to currently available analgesics, making new compounds capable of relieving chronic arthritic pain an important target of intensive drug development. One of the most important subjects of ongoing drug research involves a type of cell structure called a sodium channel. By controlling the flow of ions into and out of pain receptors (nociceptive neurons) sodium channels play a key role in the generation of pain signals. Blocking these sodium channels inhibits the transmission of pain signals from the nociceptive neurons, resulting in a localized anesthetic action and subsequent pain relief.
Several traditional Chinese herbs have been shown to demonstrate significant analgesic activity in animal studies by acting on nociceptive neurons and pain pathways to relieve pain and calm oversensitized nervous systems.
• Gastrodia root has been shown to exert novel pain relief and inflammatory-mediating activities, as well as in vivo and in vitro inhibitory activity on nitric oxide (NO) production.
• Activated Aconite exhibits especially potent analgesic properties, according to a recent study conducted by researchers with the Department of Anesthesiology, Perioperative and Pain Medicine at Harvard Medical School. Their research reveals that one of the active ingredients in aconite–Bulleyaconitine A, or BLA– strongly reduces sodium channel currents to block overactive pain signals for prolonged periods of time. In China, BLA has been approved for the treatment of chronic pain and rheumatoid arthritis.
• Scrophularia has demonstrated a powerful painkilling ability equal to that of cortisone and twice as effective as indomethacin, a popular NSAID used to treat arthritis. As with the other herbal ingredients, scrophularia exerts these significant analgesic effects with virtually no side effects.
• Notoperygium root is used in traditional medicine to relieve discomfort due to aching in the limbs and joints, especially in the upper part of the body. Recent studies reveal that Notoperygium works to support joint discomfort, in part, by inhibiting 5-Lipoxygenase (5-LOX) and COX, two key enzymes involved in the arachidonic acid pathway that constitutes one of the main mechanisms for the production of pain and inflammation.
• Eucommia bark is derived from the Eucommia, or hardy rubber tree. In traditional Chinese medicine, Eucommia bark is used to strengthen the bones and muscles and alleviate discomfort in the lower back and legs. Eucommia bark contains a substance, iridoid glycoside, that has a long history of use for inflammation.(5) One glycoside, aucubin, has been shown to be a specific inhibitor of NF-kappaB activation in mast cells, which might explain its beneficial effects.
• Chinese Ligusticum root contains alkaloids that have been shown in studies to inhibit TNF-alpha production and TNFalpha- mediated NF-kappaB activation.(7) One study conducted in Japan showed that active compounds found in Ligustici Sinensis have both anti-inflammatory and pain reducing effects, exerting its anti-inflammatory benefits in the early and the late stages of processes in the inflammatory pathology.
Chinese Herbs and Inflammation
Inflammation is the body’s front line defense against infection and damage. The five primary symptoms of inflammation – redness, heat, swelling, pain, and restriction of movement – are signs that the body is bringing in more blood and immune resources, such as white blood cells and macrophages, to remove microorganisms and other foreign matter. Redness is a sign that vasodilation is allowing more blood and other fluids to reach the affected area; local heat reflects the increased flow of warm blood from deep within the body; swelling (edema) is caused by the local accumulation of fluids; pain and restricted mobility arise from the added pressure caused by the swelling.
With osteoarthritis, inflammation is initially triggered either by trauma or irritation resulting from age-related damage to joint tissues. With the onset of inflammation the immune system responds by releasing additional pro-inflammatory factors (i.e., TNFalpha, IFN-gamma, IL-1beta, IL-2, IL-4, LTB(4), and NO) that accelerate cartilage damage. In time the cartilage begins to degrade, shedding pieces of cartilage throughout the interior joint capsule. This new “foreign” material is, in turn, targeted for destruction by the immune system, further fueling the inflammatory response as the body struggles to eliminate the cellular debris. In time this process results in the eventual destruction of the joint.
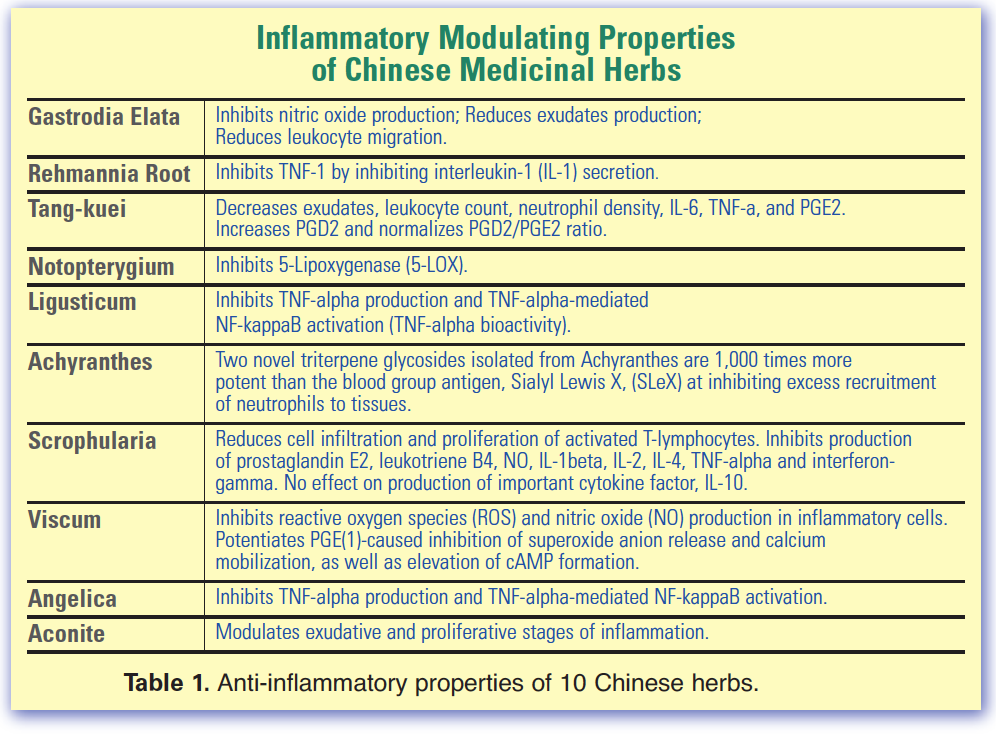
Once again a number of traditional Chinese have been shown to exhibit potent anti-inflammatory properties for both short and long-term support for countering inflammation, dampening pain, reducing swelling and stiffness, and restoring cartilage integrity (Table 1).
• Tang-kuei root has been shown to reduce edema (swelling) in early and late stages of inflammation by decreasing leukocyte counts, neutrophil density, and interleukin-6 (IL-6) expression.Tang-kuei has also been found to increase levels of PGD2, an important natural anti-inflammatory prostaglandin. Most significantly, tang-kuei is a natural source of ferulic acid, a potent antioxidant that protects cells from damaging reactive oxygen species (ROS) implicated in the pathology and progression of arthritis.
• Achyranthes (Cyathula) inhibits collagen-induced arthritis and acute edema. Most significantly, two novel triterpene glycosides isolated from achyranthes have been shown to be 1,000 times more potent than Sialyl Lewis X (SleX), an important blood group antigen that inhibits excess recruitment of neutrophils to injured tissues. This is an extremely important property. With arthritis, when too many white blood cells are recruited to an injured joint the neutrophils attack and destroy healthy tissues, leading to conditions such as septic shock and rheumatoid arthritis.
• Rehmannia contains a unique iridoid glycoside, catalpol, that has been shown to exert protective effects on dopaminergic neurons to help inhibit microglial activation, thereby reducing the production of pro-inflammatory factors.
• Scrophularia reduces edema, cell infiltration and proliferation of activated Tlymphocytes in damaged joint tissues. Additionally, scrophularia has been shown to inhibit a number of inflammatory factors, including prostaglandin E2, leukotriene B4, NO, interleukin-1beta, interleukin-2, interleukin-4, interferongamma and tumor necrosis factor-alpha (TNFa), but had no negative effect on the production of interleukin-10, a powerful anti-inflammatory cytokine. Moreover, scrophularia is the source of a unique glycoterpenoid, Verbascosaponin A, that has been shown to be twice as potent as the NSAID indomethacin for relieving inflammation and pain.
Herbs For Joint Circulation
Arthritis results in impaired blood circulation to the joints, contributing to joint deterioration, cold sensations, weakness and stiffness. Advanced arthritis also inhibits ability to engage in physical exercise, further contributing to poor limb circulation. Arthritis-related changes to blood chemistry also increase risks of developing blood clots (thrombosis) in the veins and arteries, just the type of condition aggravated by COX-2 inhibitor drugs. Contemporary research reveals several traditional herbs that have been shown to counter the negative effects of arthritic inflammation on circulation.
• Gastrodia has been shown to interact with human fibrinogen to act as a natural anticoagulant. By inhibiting interactions between fibrin molecules, gastrodia effectively inhibits the formation of arthritic-related thrombosis (blood clots) without interfering with normal clotting required for tissue maintenance.
Herbal Support for Relaxation of Joint Muscles, Collagen Synthesis
Arthritis causes painful swelling and stiffness that restricts joint movement. In time, limited movement leads to atrophy of the muscles surrounding the joints due to lack of use. Several herbs have been shown to relax arthritic joint muscles.
• Tang-kuei, in particular, has been shown in animal studies to exert a muscle relaxant effect to relax muscles and aid in restoring joint mobility.
• Eucommia has been shown to support recovery of joint mobility by promoting collagen synthesis. Researchers working with extracts of eucommia report that collagen synthesis was significantly increased when the herb was administered to laboratory rats raised to model age-related loss of joint cartilage.
Summary: Long-Term Benefits
By supporting natural pain relief through analgesic, anti-inflammatory and circulatory actions, as noted above, traditional Chinese arthritis herbs have been shown to enhance restoration of healthy joint function while reducing pain, inflammation and swelling. In addition to enhancing comfort and flexibility, many users of Chinese herbs report long-term health benefits, including improvements in memory, normalization of blood pressure levels, and antispasmodic and sedative effects.
References
1. Ahn EK, Jeon HJ, Lim EJ, Jung HJ, Park EH. Anti-inflammatory and anti-angiogenic activities of Gastrodia elata Blume. J Ethnopharmacol. 2007 Apr 4;110(3):476-82. Epub 2006 Oct 19.
2. Tian YY, An LJ, Jiang L, Duan YL, Chen J, Jiang B. “Catalpol protects dopaminergic neurons from LPS-induced neurotoxicity in mesencephalic neuron-glia cultures,” Life Sci., 2006 Dec 23. Pubmed ID: 17049947.
3. Jung SM, Schumacher HR, Kim H, Kim M, Lee SH, Pessler F. “Reduction of urate crystal-induced inflammation by root extracts from traditional oriental medicinal plants: elevation of prostaglandin D2 levels,” Arthritis Res Ther. 2007 Jul 5;9(4):R64.
4. Zschocke S, Lehner M, Bauer R. “5- Lipoxygenase and cyclooxygenase inhibitory active constituents from Qianghuo (Notopterygium incisum).” Planta Med. 1997 Jun;63(3):203-6.
5. Park KS, Chang IM. “Anti-inflammatory activity of aucubin…,” Planta Med. 2004 Aug. Pubmed ID: 15326552.
6. Jeong HJ, Koo HN, Na HJ, Kim MS, Hong SH, Eom JW, Kim KS, Shin TY, Kim HM, “Inhibition of TNF-alpha and IL-6 production by Aucubin through blockade of NF-kappaB activation RBL-2H3 mast cells,” Cytokine. 2002 Jun 7. Pubmed ID: 12161100.
7. Liu L, Ning ZQ, Shan S, Zhang K, Deng T, Lu XP, Cheng YY. Phthalide Lactones from Ligusticum chuanxiong inhibit lipopolysaccharide- induced TNF-alpha production and TNF-alpha-mediated NF-kappaB Activation. Planta Med. 2005 Sep;71(9):808-13.
8. Ozaki Y “Anti-inflammatory effect of tetramethylpyrazine and ferulic acid,” J. Chem Pharm Bull (Tokyo). 1992. Pubmed ID: 1525949
9. Han SB, Lee CW, Yoon YD, et al. “… arthritic inflammation using an oriental herbal combination BDX-1 isolated from Achyranthes bidentata and Atractylodes japonica.” Arch Pharm Res. 2005 Aug;28(8):902-8.
10. Ida Y, Satoh Y, Katsumata M, et al. “Two novel oleanolic acid saponins having a sialyl Lewis X mimetic structure from Achyranthes fauriei root.” Bioorg Med Chem Lett. 1998 Sep 22;8(18):2555-8.
11. Schinella GR, Tournier HA, Prieto JM, Mordujovich de Buschiazzo P, Ríos JL. Antioxidant activity of anti-inflammatory plant extracts. Life Sci. 2002 Jan 18;70(9): 1023-33.
12. Li YM, Han ZH, Jiang SH, Jiang Y, Yao SD, Zhu DY. Fast repairing of oxidized OH radical adducts of dAMP and dGMP by phenylpropanoid glycosides from Scrophularia ningpoensis Hemsl. Acta Pharmacol Sin. 2000 Dec;21(12):1125-8.
13. Giner RM, Villalba ML, Recio MC, Máñez S, Cerdá-Nicolás M, Ríos J. “Anti-inflammatory glycoterpenoids from Scrophularia auriculata,” Eur J Pharmacol. 2000 Feb 18;389(2- 3):243-52.
14. Wang CF, Gerner P, Wang SY, Wang GK. “Bulleyaconitine A isolated from aconitum plant displays long-acting local anesthetic properties in vitro and in vivo,” Anesthesiology. 2007 Jul;107(1):82-90. Anesthesiology. 2007 Jul;107(1):82-90.












I wish I can get in South Africa.Please direct me where to get in South Africa
..
I’m sorry Engelina, but every time we’ve tried to ship to South Africa our orders were returned.
Are there any risks of developing an allergic reaction to these herbs?
There are always risks that an individual could be allergic to a specific compound or ingredient, but in over 18 years we have yet to see a single report of an adverse event, and we maintain a stringent adverse events reporting procedure, overseen by a senior FDA consultant. Still, never say never.