Preventing Macular Degeneration, Diabetic Retinopathy and Related Ocular Disorders
By Jim English
The structure of the human eye naturally lends itself to comparison to a living camera. Light passing through the lens is focused on the retina, a tightly packed layer of light-sensitive cells (photoreceptors) arrayed across the back of the eye. Millions of photoreceptors, called rods and cones, respond to variations in color and light intensity by transmitting electrical signals to the brain where they are processed to produce what we experience as vision.
The photoreceptors of the retina expend a great deal of energy processing light and require a constant supply of oxygen, glucose, and other nutrients. Consequently the retina is supported by a dense tangle of blood vessels that supply one of the highest rates of blood flow found anywhere in the body. Unfortunately the retina is an extremely delicate structure that is vulnerable to damage from a number of sources, including oxidative damage from free radicals. The tissues of the retina are also rich in polyunsaturated fatty acids, which are particularly prone to damage from free radicals.
Macular Degeneration
Macular degeneration is a group of disorders that involve the slow destruction of the central region of the retina known as the macula. In ARMD, the macula slowly deteriorates, eventually leading to almost complete blindness of the central visual field and leaving only the very edges of peripheral vision. Most cases of macular degeneration occur in people over age sixty and are referred to as age-related macular degeneration (ARMD). ARMD is a major cause of blindness affecting up to fifteen million people over the age of sixty.
Macular degeneration causes different symptoms in different people, and in its early stages there may be few noticeable changes in vision.
Often there is only loss of vision in one eye while the other eye continues to see well for many years. But when both eyes are affected, reading and close-up work can become difficult.
ARMD, like atherosclerosis, is a disease caused by poor circulation. If blood flow is affected by atherosclerosis, diabetes, or any other age-related health problem, the macula slowly atrophies and dies. This process is further hastened by the accelerated production of free radicals that accumulate in the retina when there is reduced blood flow.
Smoking contributes to the progression of ARMD by reducing the supply of blood, narrowing the blood vessels, and thickening the blood. A high-fat, high-cholesterol diet leading to fatty plaque deposits in the macular vessels also hampers blood flow. Additionally, a shortage of antioxidants may also increase the tendency for ARMD.
Diabetic Retinopathy
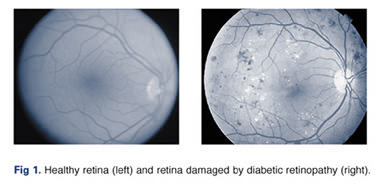
While people with diabetes are at increased risk of developing serious eye problems, such as cataracts and glaucoma, diabetic retinopathy is the number one vision threat. Diabetic retinopathy is a serious complication of diabetes that damages the small blood vessels of the retina (Fig. 1). Diabetic retinopathy affects half of all Americans diagnosed with diabetes, and if left untreated, about half of those with the advanced form, proliferative retinopathy, become blind within five years, compared to just five percent of those who receive treatment.
In the early stages of the disease, non-proliferative, or background retinopathy, the small blood vessels of the retina weaken and develop bulges (micro-aneurysms) that can leak blood into the surrounding tissues. Vision is rarely affected during this stage of retinopathy. In the advanced, proliferative stage, impaired circulation caused by damaged and narrowed blood vessels deprives the retina of oxygen. To cope with this problem the circulatory system attempts to maintain adequate oxygen levels by growing new, fragile blood vessels on the retina that can extend into the vitreous (the jelly-like substance inside the back of the eye).
These fragile vessels can rupture and release blood into the interior of the eye, leading to blurred vision or temporary blindness. This results in the formation of scar tissue that eventually pulls the retina away from the back of the eye (retinal detachment), and leads to permanent vision loss. An additional condition called macular edema can occur at any time, causing severe blurring of vision as fluid accumulates around the macula.
While all diabetics are at risk for developing diabetic retinopathy, pregnant women with diabetes are more susceptible and may require dilated eye examinations each trimester to protect their vision.
Glaucoma
According to the American Academy of Ophthalmology, over one million people in the United States are at risk for going blind because they don’t know they have glaucoma. Glaucoma is a condition marked by damage to the optic nerves (the bundle of nerve fibers that carries information from the eye to the brain) caused by elevated pressure inside the eye. It is estimated that about fifty million people worldwide suffer impaired vision, if not complete blindness, caused by glaucoma. In the United States, about 300,000 new cases are diagnosed each year, adding to the more than three million cases already on record.
Glaucoma is called the “sneak thief of sight” because it strikes without obvious symptoms.
People with glaucoma are usually unaware of it until they have a serious loss of vision. In fact, about half of those who have glaucoma do not know it. Currently, that damage cannot be reversed.
While there are usually no warning signs, some symptoms may occur in the later stages of the disease, such as a loss of peripheral vision, difficulty focusing on close work, seeing halos around lights, and frequent changes of prescription glasses. Unfortunately, though, once the vision is lost, it is gone forever.
African Americans are at a higher risk of developing glaucoma than other racial groups. Others at risk include:
- Anyone with a close relative who has glaucoma;
- Seniors;
- People with diabetes;
- People taking steroid medications for extended periods of time.
UV-Induced Eye Damage
Exposure to ultraviolet (UV) radiation produced by the sun can damage the cornea, leading to a painful condition known as photokeratitis. Ultraviolet radiation also contributes to the development of other serious eye disorders, including cataracts, degenerative corneal changes, and skin cancer around the eye.
UV actually refers to three types of ultraviolet light – UV-A, UV-B, and UV-C. The milder form of radiation, UV-C rays, are normally screened out by the ozone layer and don’t present much of an immediate health threat. The more powerful UV-A rays are composed of longer wavelength radiation that causes skin tanning and premature skin aging. UV-A rays can reach the retina, and long-term exposure may greatly increase incidence of macular degeneration. UV-B light, the active, shorter wavelengths of radiation, are responsible for blistering sunburns and skin cancer, and cause the greatest damage to eyes.
Cataracts, caused when the lens becomes cloudy, occur over a period of many years and are a major cause of visual impairment and blindness worldwide.
Studies have implicated UV radiation in the development of cataracts, and have also shown that certain types of cataracts are linked to a history of higher exposure to UV rays, especially UV-B radiation.
Since the human lens absorbs UV radiation, individuals who have cataract surgery are at increased risk of retinal damage from sunlight. And people with retinal dystrophies or other chronic retinal conditions may be at an even greater risk since their retinas may be less resilient to normal exposure levels to begin with.
Protecting Your Eyes
Age-related cataracts, glaucoma, macular degeneration, and diabetic retinopathy are among the leading causes for loss of vision. Unfortunately conventional medical approaches to preserving sight haven’t offered much hope for treatment of these blinding eye diseases and about the only option eye specialists can offer is sympathy and “watchful waiting,” while documenting their patients’ progressive loss of vision. Often laser surgery or radiation treatments are used as a last resort to temporarily stall further loss of vision once the problem has progressed to the point of imminent blindness.
As with many degenerative conditions, the best approach is a course of prevention, combined with nutrients shown in numerous clinical studies to support healthy vision. A number of nutrients have been extensively studied for their ability to treat a wide variety of vision-related conditions by preventing the damage caused by free radical activity and by enhancing the delivery of blood and oxygen to the retina to help repair tissues.
Taurine
Taurine is a sulfur-containing amino acid that stabilizes membranes, protects against free radicals, and is an ocular housekeeper, helping the macrophages in the retina eliminate debris from the photoreceptor cells. Taurine is necessary for the chemical reactions that produce normal vision, and deficiencies are associated with retinal degeneration. Besides protecting the retina, taurine may help prevent and possibly reverse age-related cataracts. When taurine is deficient, physicians often observe retinal decline. In one study of patients with primary open angle glaucoma (OAG) the fluid discharge efficacy almost doubled after treatment with taurine. In addition, taurine counterbalances excessive levels of glutamate and excitatory neurotransmitters and protects ocular tissue against oxidative stress and ischemia.
R-Lipoic Acid
A broad range of free radicals are rendered helpless by lipoic acid, a fat- and water-soluble antioxidant. Lipoic acid has been shown to prevent cataracts and diabetic nerve damage by eliminating oxidative stress, improving glucose utilization, and increasing blood flow to the nerves. In addition, lipoic acid recycles dietary antioxidants like vitamin E and raises glutathione levels. In one group of 45 patients with OAG, visual function and liquid drainage improved in approximately 50 percent of the subjects taking lipoic acid in comparison to controls. R-lipoic acid has been demonstrated to be 2-10 times more effective than lipoic acid. In a study designed to mimic the radiation exposure experienced by astronauts, jet crews and military personnel who have suffered a radiation accident, R-lipoic-acid was shown to protect against radiation-associated protein leakage in the eye lens.
Xanthophylls
Researchers have demonstrated that when eyes are exposed to intense UV light the result is extensive damage to retinal tissues, leading to a loss of photoreceptors, fragmentation of retinal cells, and extensive cell death in the macula. Xanthophylls, such as lutein, zeaxanthin and cryptoxanthin, are carotenoids that help to protect the retina from damaging exposure to sunlight, shielding up to 40 percent of damaging UV rays to help maintain ocular health.
Bilberry
Bilberry extract contains anthocyanosides, potent antioxidants that assist in maintaining the integrity of collagen structures in the eyes reducing leakage of fine capillaries in the retina. Bilberry pigment helps produce visual purple, an important chemical that helps convert light into electrical signals for the brain. Bilberry has traditionally been recommended for reducing eyestrain and improving night vision due to its ability to enhance vision in low light conditions often encountered by pilots and military personnel. Bilberry also reduces general eyestrain, which makes it particularly beneficial for students, computer operators, and anyone who must use their eyes for long periods without rest.
Quercetin
Quercetin is a plant phytochemical (flavonoid) similar to, and in some ways, more powerful than vitamin C. Quercetin prevents the vascular damage caused by LDL oxidation, shields the eye against free radicals, modulates nitric oxide production and prevents collagen breakdown.
N-Acetyl Cysteine
N-Acetyl Cysteine (NAC) is the pre-acetylized form of the simple amino acid Cysteine. NAC is a powerful antioxidant and a premier antitoxin and immune support substance. In the eye NAC scavenges reactive intermediates, guards against the toxicity of nitric oxide, and lessens oxidant injury.
Ginkgo Biloba
Ginkgo biloba is a potent free radical scavenger that supports healthy vision by preventing free radical damage commonly seen in eye diseases such as macular degeneration. A number of experimental studies suggest that ginkgo extracts are potentially useful for treating retinal damage induced by a variety of disorders. When German scientists tested ginkgo’s protective effects on the retinas of twenty-five older people they found that the herb dramatically improved vision in all subjects after only four weeks of treatment. According to the researchers, ginkgo caused a “significant increase in retinal sensitivity.”
Scientists speculated that ginkgo extract might also slow the progression of ARMD by increasing blood flow to the retina and by halting the free radical damage to the photosensitive cells.
In one double-blind trial twenty volunteers were given either 160 mg of ginkgo extract, or a placebo pill, every day for six months. At the end of the study, the group receiving ginkgo showed significant improvements in their long distance visual focus. There was no improvement in the group receiving the dummy pill.
Ongoing studies also show that the greater the damage to retinal tissues, the more profound an effect the ginkgo has on improving vision. These studies show that ginkgo is not only effective in improving vision but, in cases where the vision is damaged by poor circulation, the damage can be significantly reversed.
Human studies also support the use of ginkgo extract in treating diabetic retinopathy. In one double-blind trial, researchers gave daily doses of 160 mg of a standardized ginkgo extract to a small group of people with mild diabetic retinopathy. After six months, these volunteers had a noticeable improvement of their pre-existing impaired vision. In addition, it is suspected that ginkgo’s ability to inhibit the platelet-activating factor (PAF), is involved in protecting eye tissues from retinopathy, since ginkgolide B, a known PAF antagonist, has been shown to reduce experimentally induced retinal lesions in animals.
In 1999, researchers tested the therapeutic effects of ginkgo extract on people with glaucoma. Eleven healthy volunteers were treated with either 40 mg of ginkgo extract, or a placebo, three times daily for two days. By measuring blood flow in the eyes before and after treatment, the researchers found a significant increase in blood flow in the main eye artery in those receiving ginkgo, but no change was noted in the placebo group. The results indicate that ginkgo effectively increased the blood flow in the eyes, which helped lower the intraocular pressure, thereby slowing the progression of the disease.
Carnosine
Carnosine is a naturally-occurring dipeptide that has demonstrated efficacy in treating a variety of ophthalmic conditions, including corneal diseases, cataracts as well as glaucoma and increased intraocular pressure. In 1997, clinical trials were conducted in 109 ophthalmic patients with carnosine-containing eye drops. The results confirmed accelerated healing of corneal erosions, trophic keratitis, post-herpetic epitheliopathy, primary and secondary corneal dystrophy and bullous keratopathy. Most striking, however, was the ability of carnosine to eliminate existing cataracts.
Furthermore, carnosine is thought to function as a “molecular water pump.” In earlier experiments it was demonstrated that applying carnosine to the conjunctiva (the membrane covering the eye) caused a decrease in normal intraocular pressure and reduced prostaglandin-induced ocular hypertension (related to glaucoma).
Conclusion
While sometimes referred to as “windows into the soul,” eyes in fact can reveal much about our general state of health. Many of the nutrients discussed here work together to offer a wide range of health benefits to protect these exquisite structures and help preserve vision – and general health – for a lifetime.
References
1. Lebuisson DA, Leroy L, Rigal G. Treatment of senile macular degeneration with Ginkgo biloba extract. A preliminary double-blind, drug versus placebo study. Presse Med. 1986; 15:1556-58.
2. Schalch W. Carotenoids in the retina – A review of their possible role in preventing or limiting damage caused by light and oxygen. EXS (Supplementum to Experientia). 1992; 62:280-298.
3. Lake N, Malik N. Retinal morphology in rats treated with a taurine transport antagonist. Exp Eye Res. 1987; 44:331-46.
4. Filina AA, Davydova NG, Kolomoitseva EM. The effect of lipoic acid on the components of the glutathione system in the lacrimal fluid of patients with open-angle glaucoma. Vestn Oftalmol. 1993;109(5):5-7.
5. Mizushima S, Nara Y, Sawamura M, Yamori Y. Effects of oral Taurine supplementation on lipids and sympathetic nerve tone. Adv Exp Med Biol. 1996;403:615-22.
6. Trachtman H, Futterweit S, Maesaka J, Ma C, Valderrama E, Fuchs A, Tarectecan AA, Rao PS, Sturman JA, Boles TH, et al. Taurine ameliorates chronic streptozocin-induced diabetic nephropathy in rats. Am J Physiol. 1995;269(3 Pt 2):F429-38.
7. Maitra I, Serbinova E, Tritschler HJ, Packer L. Stereospecific effects of R-lipoic acid on buthionine sulfoximine-induced cataract formation in newborn rats. Biochem Biophys Res Commun. 1996 Apr 16;221(2):422-9.
8. Bantseev V, Bhardwaj R, Rathbun W, Nagasawa H, Trevithick JR. Antioxidants and cataract: (cataract induction in space environment and application to terrestrial aging cataract). Biochem Mol Biol Int. 1997 Sep;42(6):1189-97.
9. Lebuisson DA, et al. Treatment of senile macular degeneration with Ginkgo biloba extract. A preliminary double-blind, drug versus placebo study. Presse-Medicale, 1986;15:1556-1558.
10. Lebuisson, D.A., Leroy, L., Rigal, G. Treatment of senile macular degeneration with Ginkgo biloba extract. Presse-Medicale, 1986, 15: 1556-1558.
11. Baslow, MH. Function of the N-acetyl-L-histidine system in the vertebrate eye. Evidence in support of a role as a molecular water pump. J Mol Neurosci, 1998, 10(3), 193-208.
12. Maichuk, IUF, Formaziuk, VE, Sergienko, VI. Development of carnosine eyedrops and assessing their efficacy in corneal diseases. Vestn Oftalmol, 1997, 113(6): 27-31.
13. Yuneva, M.O., Bulygina, E.R., Gallant, S.C., et al. Effect of carnosine on age-induced changes in senescence-accelerated mice. J Anti-Aging Medicine, 2: 1999, 337-342.












Absolutely! Unless you have a medical or eye problem that requires frequent attention.
I agree! Protect your eyes with lenses that block both UVA and UVB light, and avoid smoking. It’s important to control your blood pressure, watch your weight and manage diabetes as well.