A study in the Archives of Internal Medicine (Guyton, et al, 2000) confirms my long-held belief in the superiority of niacin (vitamin B3) as a lipid-lowering agent. A proprietary timed-release version of niacin (Niaspan) was compared to the pharmaceutical drug gemfibrozil (Lopid). The study involved 399 male and female subjects ranging in age from 21 to 75, all of whom had low levels of HDL (high density lipoproteins — “good cholesterol”) less than 40 mg/l.
Other criteria for inclusion in this study were triglycerides less than 400 mg/l, and LDL (low density lipoproteins—“bad cholesterol”) less than 260 mg/l. Niacin was administered once daily at bedtime. The niacin dosage was begun at 375 mg/day, and then increased progressively over the course of the study, and maintained at a level of 2,000 mg nightly for 8 weeks. The duration of the study was 16 weeks. Subjects took an aspirin as-needed to prevent flushing. Gemfibrozil 600 mg was administered twice daily over the entire 16 weeks.
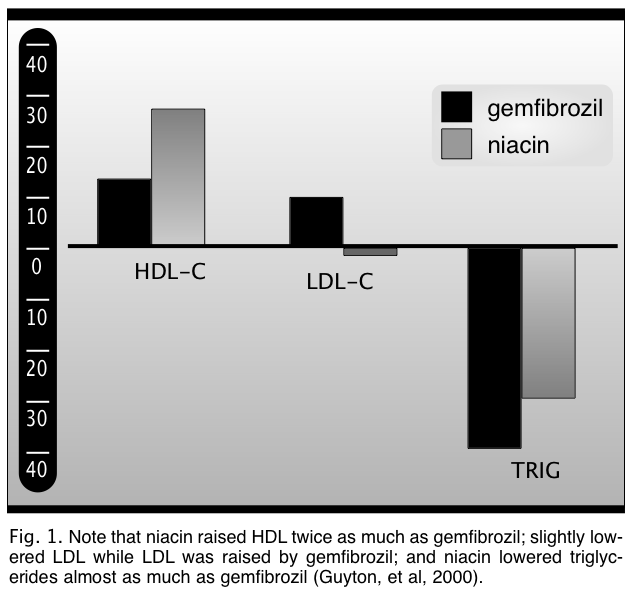
Niacin increased HDL levels over 25%, compared to an increase of 13.3% due to gemfibrozil. Gemfibrozil actually raised LDL (the “bad” cholesterol, remember?), while niacin slightly lowered this fraction. Gemfibrozil lowered triglyceride levels by 40%, compared to a 30% decrease from niacin. Thus, niacin resulted in an overall improvement in the lipid profile which exceeded that induced by gemfibrozil (Fig. 1).
However, niacin favorably altered several other cardiovascular risk factors as well. Apolipoprotein (a) levels were significantly (20%) reduced by niacin, but were not altered by gemfibrozil. Both substances reduced serum apolipoprotein (b) levels by the same amount. Fibrinogen, a third risk factor, was reduced by niacin, but increased 6-9% by gemfibrozil. The authors concluded, “Niaspan, 2,000 mg, had a significantly better effect on fibrinogen levels than gemfibrozil.”
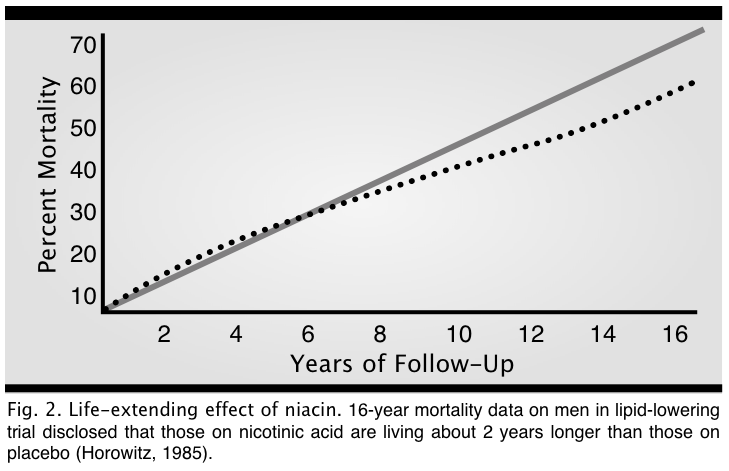
These results support many previous studies on the use of niacin as a lipid-lowering nutrient. For example, in the Coronary Drug Project, which enrolled men with a previous myocardial infarction, niacin use resulted in a 26% decrease in second non-fatal heart attacks over a six-year period, and an 11% decrease in total mortality after 15 years of followup (Canner, et al, 1986) (Fig. 2).
Niacin Stimulates Growth Hormone
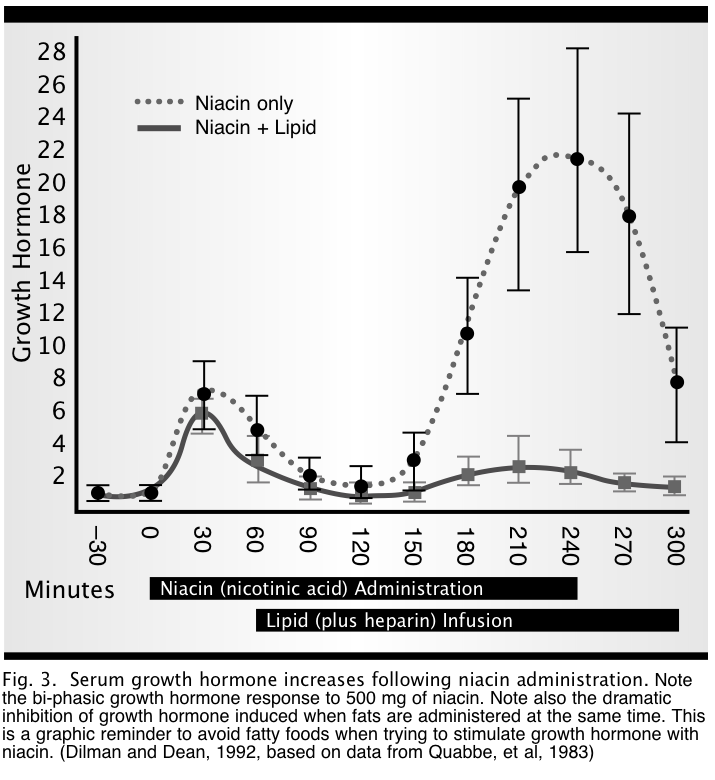
While extolling the benefits of niacin, one frequently overlooked “side effect” is that niacin is a powerful releaser of growth hormone (Quabbe, et al, 1983) (Fig. 3). Quabbe and colleagues administered 500 mg niacin intravenously to humans, and noted a dramatic rise in growth hormone. In a second phase of their study, they simultaneously administered an infusion of fatty acids. Note that the fat completely blunted any rise in growth hormone. The practical take-home lesson of this study is that anyone using niacin as a growth hormone stimulant should take it on an empty stomach (glucose and insulin also inhibit growth hormone, as well as fatty acids).
Side Effects and Contraindications to High-Dose Niacin
High dose niacin is very safe. Its most frequent “adverse effect” is a harmless flushing of the skin, accompanied by itching. This effect usually resolves over a few days or weeks of use. Taking an aspirin 30 minutes or so before the niacin also helps to reduce this effect. Another way to minimize the flushing is to start with low doses (50-100 mg) and gradually increase the dose as tolerated. Finally, inositol hexanicotinate (IHN)—another non-flushing form of niacin—can also be used. IHN, while a bit more costly than niacin, is effective in somewhat lower doses, thereby remaining cost effective. Another side effect is the potential for elevation of liver enzymes or liver toxicity. Liver toxicity is rare, and occurs most frequently with timed release preparations.
Anyone contemplating high dose niacin therapy probably should have their liver enzymes checked within several months of achieving therapeutic levels (1,500-3,000 mg). The only absolute contraindication to niacin therapy is insulin-dependent diabetes. Niacin aggravates blood sugar problems in insulin dependent diabetics, further worsening their lipid problems, usually causing their triglycerides to skyrocket. Alternatively, I recommend niacinamide (also contained in Optimum D) in doses up to three grams daily for insulin dependent diabetics. Although niacinamide does not normally effect lipid levels in non-diabetics, because of its glucose-stabilizing affect in diabetics, it tends to normalize their blood lipids—especially, the triglycerides.
Conclusion
Niacin once again emerges as a low-cost, highly effective agent to reduce cholesterol, raise HDL, and lower LDL and triglycerides. In addition, it has the added benefits of lowering apolipoproteins a and b, and fibrinogen, and raising growth hormone. Muntoni (1974) stated that “lipostatic” substances are the agents of choice to retard aging, and niacin may very well be the best substance in this class (Dilman and Dean, 1992).
References
Canner, P.L., Berge, K.G., Wenger, N.K., et al. Fifteen year mortality in Coronary Drug Project patients: long-term benefit with niacin. J Am Coll Cardiol, 1986, 8: 1245-1255.
Dilman, V., and Dean, W. The Neuroendocrine Theory of Aging and Degenerative Disease, 1992, The Center for Bio-Gerontology, Pensacola.
Guyton, John R., Blazing, Michael A., Hagar, James, et al. Extended-release niacin vs Gemfibrozil for the treatment of low levels of high density lipoprotein cholesterol. Arch Intern Med, 2000, 160: 1177-1184.
Horowitz, N. Link niacin to longevity after an MI. Medical Tribune, 1985, 26: 12, pp. 1, 17.
Muntoni, S. Inhibition of fatty acid oxidation by biguanides: implication for metabolic physiopathology. Adv Lipid Res, 1974, 12: 311-377.
Quabbe, H.J., Ramek, W., and Luyckx, A.S. Growth hormone, cortisol and glucagon concentration during plasma free fatty acid depression. Different effects of nicotinic acid and an adenosine derivative. J Clin Endocr Metab, 1983, 57: 410-414.















[…] chcesz mocniej wgłębić się w temat, polecam przeczytanie tego artykułu, w którym znajdziesz odnośniki do konkretnych badań […]
[…] activity and is known to help balance cholesterol. It also assists brain function and aids the secretion of human growth hormone […]
However, niacin favorably altered several other cardiovascular risk factors as well. Apolipoprotein (a) levels were significantly (20%) reduced by niacin, but were not altered by gemfibrozil. Both substances reduced serum apolipoprotein (b) levels by the same amount. Fibrinogen, a third risk factor, was reduced by niacin, but increased 6-9% by gemfibrozil. The authors concluded, “Niaspan, 2,000 mg, had a significantly better effect on fibrinogen levels than gemfibrozil.”
Niacyna po raz kolejny pojawia się jako tani, bardzo skuteczny środek do obniżania poziomu cholesterolu, podnoszenia poziomu HDL oraz obniżania poziomu LDL i trójglicerydów. Ponadto ma dodatkowe zalety polegające na obniżeniu apolipoprotein aib, fibrynogenu i podniesieniu hormonu wzrostu.
Niacyna po raz kolejny pojawia się jako tani, bardzo skuteczny środek do obniżania poziomu cholesterolu, podnoszenia poziomu HDL oraz obniżania poziomu LDL i trójglicerydów. Ponadto ma dodatkowe zalety polegające na obniżeniu apolipoprotein aib, fibrynogenu i podniesieniu hormonu wzrostu