You’re up in the mountains, the snow is blindingly white, and the sun is blazing down from the sky: ideal skiing conditions – but any skiers carrying the herpes virus might also have to reckon with the onset of cold sores after their day out. Increased exposure to UV radiation releases free radicals in the body. These put the body under oxidative stress, which weakens the immune system. And that in turn allows the herpes virus to prosper.
Oxidative stress has become a major topic; not only is it implicated in many diseases, it may even be one of their causes. Other environmental influences besides UV radiation can also increase oxidative stress on the body, including air pollution, smoking and the consumption of alcohol, and not least infections. Again and again, the talk is of fighting these free (oxygen) radicals by supplementing our diet with the appropriate vitamins.
T Cells Divide After Contact With The Enemy
Researchers working with Manfred Kopf, a professor at ETH Zurich’s Institute of Molecular Health Sciences, took these questions as their starting point and have now identified a phenomenon that explains the effects of oxidative stress on immune cells.
Whenever a foreign body such as a virus or other pathogen enters our bodies, a certain class of immune cells – the T cells – jump into action, proliferating rapidly. One sub-class of these cells, the CD8+ T cells, eliminate the virus by killing cells it has infected. Other T cells, known as CD4+ T cells, coordinate the immune response to all kinds of pathogens. These are the generals in the immune system’s army.
But a week can pass before these T cells start to take their toll on a virus, because in the early stages of an infection too few T cells are able to recognise the specific pathogen. Only once they have had “enemy contact” do these few “scout” cells begin to divide, forming “clones” of themselves. With cells dividing every eight to twelve hours, it takes a few days to gather a strike force of cells in the hundreds of thousands: enough to overwhelm the infection.
No Immune Response Without a Repair Kit
However, this immune response does not work if significant oxidative stress is damaging the T cells and depriving the body of the tools it needs to repair them, as Kopf’s research group with doctoral student Mai Matsushita as lead author have now shown in their new publication in the Journal of Experimental Medicine.
If the immune cells lack repair enzyme Gpx4 (or it is defective), the T cells die off as they divide, which means the immune system cannot eliminate the pathogen and the infection becomes chronic. This is the enzyme responsible for repairing oxidative damage to the cell membrane.
Vitamin E Comes to the Rescue
To their astonishment, when testing mice whose immune cells lacked the repair enzyme, the researchers were able to save the immune cells from cell death by mixing a high dose of vitamin E into the animals’ food. That was enough antioxidant to protect the T cells’ cell membranes from damage, so they could multiply and successfully fend off the viral infection. At 500 milligrams per kilogram of mouse feed, this quantity of vitamin E was ten times higher than was present in the standardised normal food.
The researchers demonstrated this by way of a mouse model using animals in which the Gpx4 gene can be deactivated either cell-specifically or at a chosen point in time. These mice were developed by researchers at the Helmholtz Zentrum München. The ETH scientists then altered the mouse line so that the Gpx4 gene was inactive only in T cells or certain phagocytes.
Vitamin Supplements Disputed
“The benefit of vitamin tablets is a controversial topic,” says Manfred Kopf. With little scientific evidence as yet making a strong case for vitamin supplements, he felt their study was all the more interesting because it proved the effectiveness of vitamin E: “Our work shows that even a genetic defect in a major part of a cell’s antioxidative machinery can be compensated for by delivering a high dose of vitamin E. That is new and surprising.”
Kopf considers it significant that immune cells suffer the same type of death as certain kinds of cancer cells when treated with a cytostatic drug, and judges this fact to be of scientific value. Known as ferroptosis, this type of programmed cell death was first described in a scientific publication in 2012. “We are the first to demonstrate that oxidative stress causes immune cells to suffer the same type of death as cancer cells,” he says.
What Kopf isn’t yet sure of is what impact the results of their study will have on human health. He finds that people with a normal level of health and a balanced diet shouldn’t need vitamin supplements. But a supplement of vitamin E or other liposoluble antioxidants could well make sense in the event of oxidative stress, which can arise in everyday situations such as an infection or exposure to UV light. Patients with certain neurodegenerative diseases or diabetes suffer massive oxidative stress, and in these cases antioxidants could be a worthwhile addition to their treatment. How high the dose should be is something Kopf cannot say on the basis of the results of this study. It is not something they analysed, given that the research was conducted using a mouse model.
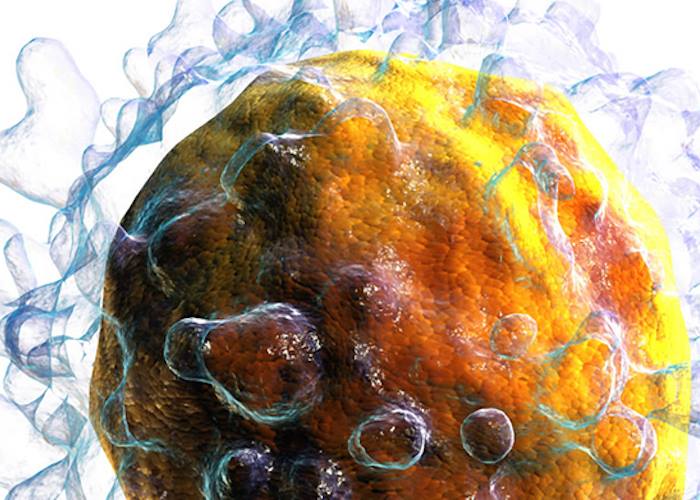
Image: A white blood cell, also known as a T cell, carries special structures on its surface with which to recognise specific pathogens. Credit: Blausen.com, CC BY 3.0 via Wikimedia Commons
Source: M. Matsushita, S. Freigang, C. Schneider, M. Conrad, G. W. Bornkamm, M. Kopf. T cell lipid peroxidation induces ferroptosis and prevents immunity to infection. Journal of Experimental Medicine, 2015; 212 (4): 555 DOI: 10.1084/jem.20140857
Journal Link: http://jem.rupress.org/