In recent years vitamin D deficiency has been linked to type 2 diabetes and heart disease, two illnesses that commonly occur together and are the most common cause of illness and death in Western countries. Both disorders are rooted in chronic inflammation, which leads to insulin resistance and the buildup of artery-clogging plaque. Now, new research in mice at Washington University School of Medicine in St. Louis suggests vitamin D plays a major role in preventing the inflammation that leads to type 2 diabetes and atherosclerosis. Further, the way key immune cells behave without adequate vitamin D may provide scientists with new therapeutic targets for patients with those disorders.
Studying mice that lacked the ability to process vitamin D in immune cells involved in inflammation, the researchers found that the animals made excess glucose, became resistant to insulin action and accumulated plaques in their blood vessels.
“The finding that vitamin D helps regulate glucose metabolism may explain previous epidemiological studies identifying an increased risk of diabetes in patients with vitamin D deficiency,” said senior investigator Carlos Bernal-Mizrachi, MD, associate professor of medicine and of cell biology and physiology. “In our study, inactivation of the vitamin D receptor induced diabetes and atherosclerosis, so normalizing vitamin D levels may have the opposite effect.”
In addition, he said inadequate vitamin D turned immune cells into transporters of fat. That may help researchers better understand how diabetes and atherosclerosis are linked and provide new possibilities for therapy.
For years, researchers have been studying vitamin D’s possible roles in inflammation and inflammatory diseases, such as type 2 diabetes and atherosclerosis. By engineering mice without the vitamin D receptor on important immune cells called monocytes and macrophages, the researchers were able to learn how those conditions are linked, according to Bernal-Mizrachi.
Monocytes are white blood cells made in the bone marrow that circulate in the bloodstream. After a few days, they typically move into the body’s tissues where they mature into cells called macrophages.
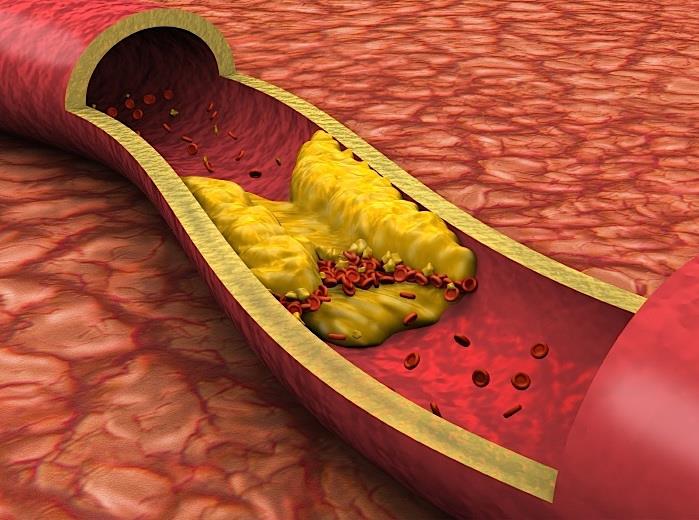
“Inactivating the vitamin D receptor on monocytes and macrophages promotes inflammation of the liver and in artery walls,” he said. “It also increases the ability of monocytes in the blood to adhere and migrate into blood vessel walls, where they deposit cholesterol and secrete inflammatory substances that lead to diabetes and heart disease.”
He said the findings suggest that getting enough vitamin D may reduce those properties in immune cells, decreasing inflammation and reducing the onset of a combination of heart disease and diabetes, which is often referred to as cardiometabolic disease. In addition, the researchers found that without vitamin D, monocytes carried fat to the walls of blood vessels, which is something that hadn’t been observed previously.
“We knew that when monocytes matured and became macrophages, they would eat cholesterol deposited inside the blood vessel wall,” said co-first author Amy E. Riek, MD, assistant professor of medicine. “But in these experiments, we found that when they don’t have vitamin D, the monocytes, while they’re still in circulation, also eat up cholesterol and carry it in the bloodstream.”
That’s an important discovery, Riek explained, because it’s much easier to find treatments that target something in the blood than it is to target the same cells after they move into the wall of a blood vessel.
“So that provides us, potentially, with a new target for therapy,” she said.
It also changes the way that scientists think about how lipids are carried into the blood vessel wall to cause plaques. Scientists already knew that LDL, the so-called bad cholesterol, carried fat deposits to the vessel wall. Now this study suggests that when monocytes don’t have enough vitamin D, they can do it, too.
“The monocytes were laden with fat in the absence of vitamin D receptor,” Bernal-Mizrachi said. “And they carried that fat into the artery, so that’s a new understanding of another way fat may get into blood-vessel walls in patients who are vitamin D deficient.”
Interestingly, the problem was reversible in the mice. When the animals that had developed type 2 diabetes and atherosclerosis received bone marrow transplants from mice with healthy vitamin D receptors on their monocytes and macrophages, their inflammation levels decreased, and the animals had lower blood glucose and became more sensitive to insulin.
Currently, Bernal-Mizrachi and Riek are conducting clinical studies in people who have type 2 diabetes, treating them with vitamin D to see whether it can prevent some of the complications of diabetes and inflammation in humans, too.
“As part of that study, we’re actually isolating monocytes from the blood of patients before and after vitamin D therapy,” Riek said. “So we can look at the inflammatory properties of those cells to see whether vitamin D is causing any changes.”
Source: Jisu Oh, Amy E. Riek, Isra Darwech, Katsuhiko Funai, Jiansu Shao, Kathleen Chin, Oscar L. Sierra, Geert Carmeliet, Richard E. Ostlund Jr., Carlos Bernal-Mizrachi. Deletion of Macrophage Vitamin D Receptor Promotes Insulin Resistance and Monocyte Cholesterol Transport to Accelerate Atherosclerosis in Mice. Cell Reports, 2015 DOI: 10.1016/