by Jim English
The human requirement for vitamins, minerals and other nutrients remains relatively constant throughout adult life. Unfortunately our ability to properly digest food and absorb vital nutrients declines with advancing age. Surprisingly, one of the most common age-related causes of impaired digestive function is the reduction of hydrochloric acid produced by the stomach.
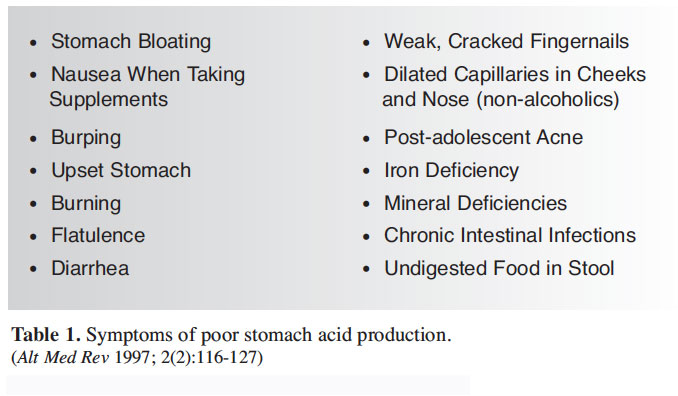
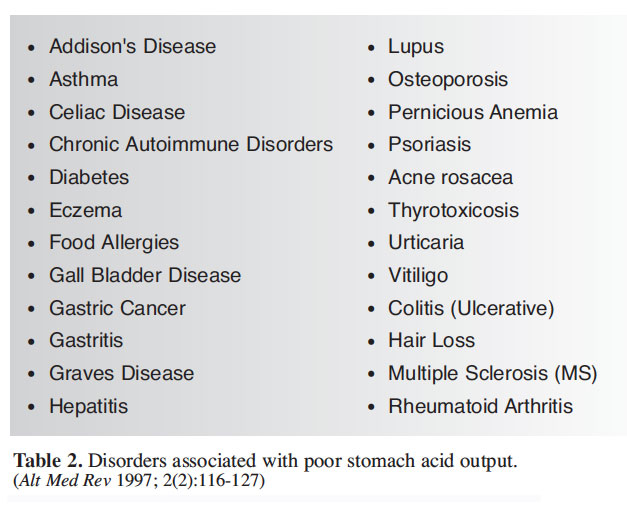
Hydrochloric acid (HCl) is an important gastric secretion that enables the body to break down proteins, activate important enzymes and hormones, and protect against bacterial overgrowth in the gut. Achlorhydria (the complete absence of stomach acid) and hypochlorhydria (low stomach acid) are common digestive problems. Symptoms of low stomach acid include heartburn, indigestion and bloating, among others (Table 1). Additionally, a number of chronic health conditions are correlated with impaired acid secretion, including allergies, asthma and gallstones (Table 2).
HCl and Digestion
Digestion is a complex body function that starts when food enters the mouth and continues as material is processed and passed on to the stomach, small intestine and large intestine. In the stomach, digestion begins with the release of a number of gastric secretions, including HCl, pepsinogen and a protective mucus coating. Secretion of hydrochloric acid and pepsin is a prerequisite for healthy digestion. Normally the stomach contains enough free hydrochloric acid (HCl) to maintain a constant stomach acidity of between pH 1 and 2. The amount of HCl produced increases rapidly following the ingestion of food. HCl has an important role in the digestion and absorption of a number of nutrients, including:
• Protein: HCI initiates the digestion of protein in the stomach by converting pepsinogen into the proteolytic enzyme, pepsin. Once formed, pepsin acts to break proteins into smaller peptides that can be absorbed by the small intestine. Without adequate gastric secretions, incompletely digested macromolecules can be absorbed into the systemic circulation.
• Carbohydrates and Fats: HCl supports the digestion and absorption of carbohydrates, fats, and vitamins A and E by stimulating the release of pancreatic enzymes and bile into the small intestine.
• Vitamins and Minerals: HCl also aids in the absorption and assimilation of vitamins and minerals such as folic acid, ascorbic acid, beta-carotene and iron, by increasing their bioavailability and effecting their release from food. Jonathan Wright, MD, Medical Director of the Tahoma Clinic, reports observing that a number of minerals and micro-trace elements are poorly absorbed in cases of low stomach acid, including calcium, magnesium, zinc, copper, chromium, selenium, manganese, vanadium, molybdenum and cobalt. (1)
Protection from Pathogens
In addition to breaking down and absorbing vital nutrients, HCl also plays an important role in maintaining a sterile environment in the stomach. HCl does this by protecting against orally ingested pathogens and acting as a barrier to prevent bacterial or fungal overgrowth of the small intestine. Researchers have shown that a common pathogen, E. coli (Escherichia coli) is inactivated when stomach acidity is high, with a pH ranging between 1.5 and 4.0. (2)
Conversely, low stomach acidity is associated with the rapid invasion of microorganisms from the colon, leading to gastric and intestinal bacterial colonization and overgrowth. (3) And in tests where researchers induced a temporary state of low acid (pH greater than 4.0) all subjects experienced bacterial overgrowth in the proximal small intestine. (4) Conversely, E coli is not found in the gastric contents of patients with achlorhydria following treatment with HCl. (5)
An additional finding of a Japanese team was a strong correlation between low stomach acidity and increased infection by Helicobacter pylori (H. pylori), (6) one of the most common chronic bacterial infections of humans and recognized as a major cause of gastritis, gastric ulcer disease, gastric carcinoma and B-cell gastric lymphoma. (7)
Low Stomach Acid and Age
Numerous studies have shown that hydrochloric acid secretion declines with advancing age (Fig. 1). In one study US researchers found that over 30 percent of men and women past the age of 60 suffer from atrophic gastritis, a condition marked by little or no acid secretion. (8) A second study found that up to 40% of postmenopausal women have no basal gastric acid secretions. (9)
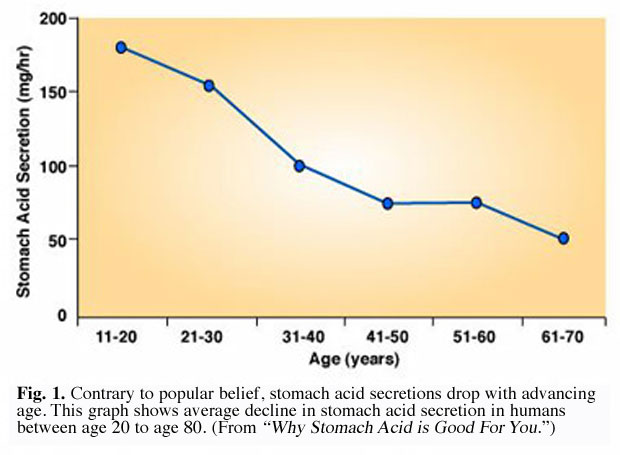
In a second study involving 3,484 subjects, researchers found that among both males and females, 27% suffered from achlorhydria, with the greatest incidence (39.8%) occurring in females aged 80 to 89 years. (10)
Researchers in Japan have also measured a similar age-related drop in gastric acidity in elderly Japanese subjects. In 1984 researchers found that 60 percent of Japanese men and women over 50 years age suffered from achlorhydria. New research based on data collected from 1989 to 1999 continued to substantiate a substantial age-related decrease in stomach acid production, though the total percentage of achlorhydric subjects dropped from 60 percent to 40 percent. (7)
Conditions of Low Stomach Acid
Symptoms of low stomach acid frequently occur several hours after eating and can include a desire to eat when not hungry, a sense of fullness after meals, flatulence, constipation and diarrhea. Symptoms that may persist regardless of eating food can include feeling soreness and burning of the mouth. (10)
Heartburn
Heartburn, a burning sensation in the chest caused by the regurgitation of bile through the stomach into the lower esophagus, is a frequent symptom of low gastric acid. The traditional approach of treating heartburn is to suppress gastric acid by taking antacids or alkalizers. This approach is the opposite of what should often be done, and in many cases only worsens the problem by suppressing gastric acidity when it is needed and promoting it (rebound phenomenon) when it is unnecessary.
Jonathan Wright, MD, states, “In 24 years of nutritionally oriented practice, I’ve worked with thousands of individuals who’ve found the cause of their heartburn and indigestion to be low stomach acidity. In nearly all of these folks, symptoms have been relieved and digestion improved when they’ve taken supplemental hydrochloric acid and pepsin capsules. (Certainly it would be preferable that our stomach production of hydrochloric acid and pepsin be restored on its own, but a reliable way to do this hasn’t been found.)” (11)
Supplemental Hydrochloric Acid
Hydrochloric acid was routinely prescribed for many symptoms and clinical conditions for over 100 years. Use of HCl by the medical establishment began to decline in the late 1920s. The decline in HCl replacement therapy, according to Jonathan Wright, was due to poorly designed and misinterpreted research that convinced medical practitioners that HCl and pepsin replacement therapy was not necessary.
“Encouraged by the legal drug industry, medical students are not taught that hypochlorhydria (inadequate stomach acid production) is treatable only with unpatentable, natural replacement therapies. Instead, their education concentrates on hyperchlorhydria (excess stomach acid production) and its treatment with patentable acid blocker drugs and highly profitable over-the-counter antacids.” (11)
Hydrochloric acid has been shown to be effective in relieving symptoms associated with achlorhydria and hypochlorhydria. Substances shown to support healthy acid secretion and digestion include:
• Betaine hydrochloride (HCl) is a nutritional supplement that has been used for over 100 years to safely restore normal gastric acidity and to support healthy gut function. Betaine HCl should not be confused with another popular nutritional supplement, anhydrous Betaine, a methyl-donor nutrient taken to control homocysteine levels.
• Pepsin has a long history of medicinal use and is considered very safe when administered to assist digestion, typically in conjunction with hydrochloric acid.
• Peppermint is used to aid the various processes of digestion due to its antibacterial and gastric-acid-promoting effects. Peppermint also aids digestive function by combating gas, increasing the flow of bile, and healing the stomach and liver. The spasmolytic property of peppermint has been found to decrease the tone of the lower esophagus sphincter so that the escape of air is made easier, which is particularly useful for relieving discomfort caused by spasms in the upper digestive tract. (12)
• Gentian: The bitter principles of the dried root of Gentiana lutea have been used in Europe as a digestive aid for centuries, especially in Swedish bitters. Gentian roots were historically used topically to treat skin tumors, and internally to treat fever and diarrhea. (13) Modern research has shown that gentian, which contains two of the most bitter substances known, the glycosides gentiopicrin and amarogentin, acts on taste bud receptors to stimulate the secretion of saliva in the mouth and hydrochloric acid in the stomach. (14)
Summary
Healthy digestion and absorption of nutrients is dependent upon the secretion of gastric acid. When gastric secretions are reduced the result can lead to nutritional deficiencies and a variety of chronic disorders. Low secretion of gastric acid can also allow orally-ingested pathogens to prevail and contribute to their overgrowth in the stomach and small intestine. HCl supplementation is a safe and effective means of restoring normal gastric levels, particularly in cases where age or chronic conditions indicate that nutrients, particularly B vitamins and minerals, are not being properly utilized.
References
1. Wright JV. Treatment of childhood asthma with parenteral vitamin B12, gastric re-acidification, and attention to food allergy, magnesium and pyridoxine. Three case reports with background and an integrated hypothesis. J Nutr Med 1990;1:277-282.
2. Takumi K, de Jonge R, Havelaar A. Modeling inactivation of Escherichia coli by low pH: application to passage through the stomach of young and elderly people. J. Appl Microbiol 2000 Dec;89(6):935-43.
3. Saltzman JR, Kemp JA, Golner BB, et al. Effect of hypochlorhydria due to omeprazole treatment or atrophic gastritis on protein bound vitamin B12 absorption. J Amer Coll Nutr 1994;13:584-591.
4. Tang G, Serfaty-Lacrosniere C, Camilo ME, et al. Gastric acidity influences the blood response to a B-carotene dose in humans. Am J Clin Nutr 1996;64:622-626.
5. Brummer P, Kasanen A. The effect of hydrochloric acid on the indican metabolism in achlorhydria. Acta Medica Scan 1956;155:11-14.
6. Morihara M, Aoyagi N, Kaniwa N, Kojima S, Ogata H.Assessment of gastric acidity of Japanese subjects over the last 15 years. Biol Pharm Bull 2001 Mar;24(3):313-5.
7. Young DG. A stain for demonstrating Helicobacter pylori in gastric biopsies. Biotech Histochem 2001 Jan;76(1):31-4.
8. Krasinski SD, Russell RM, Samloff IM, Jacob RA, Dallal GE, McGandy RB, Hartz SC. Fundic atrophic gastritis in an elderly population. Effect on hemoglobin and several serum nutritional indicators. J Am Geriatr Soc. 1986 Nov;34(11):800-6.
9. Grossman MI, Kirsner JB, Gillespie IE. Basal and histalog-stimulated gastric secretion in control subjects and in patients with peptic ulcer or gastric cancer. Gastroenterology 1963;45:15-26.
10. Sharp GS, Fister HW. The diagnosis and treatment of achlorhydria: ten-year study. J Amer Ger Soc 1967;15:786-791.
11. Jonathan Wright, MD, The Digestive Theory of Aging, Part I, http://www.tahoma-clinic.com/aging.shtml.
12. Schilcher, H,: Deutshe Apotheker Zeitung 124:1433-1443 (1984) (Brundesanzeiger (Cologne, Germany): Nov. 30, 1985; March 13, 1986.
13. Duke JA. CRC Handbook of Medicinal Herbs. Boca Raton, FL: CRC Press, 1985.
14. Bradley PR, ed. British Herbal Compendium (Vol. 1): A handbook of scientific information on widely used plant drugs. Guilford and King’s Lynn, Great Britain: Biddles Ltd; 1992:109-111.












[…] [ix] English J. Gastric Balance: Heartburn Not Always Caused by Excess Acid. Nutrition Review. April 22 2013. Accessed April 24 2014. https://nutritionreview.org/2013/04/gastric-balance-heartburn-caused-excess-acid/ […]
[…] [ix] English J. Gastric Balance: Heartburn Not Always Caused by Excess Acid. Nutrition Review. April 22 2013. Accessed April 24 2014. https://nutritionreview.org/2013/04/gastric-balance-heartburn-caused-excess-acid/ […]
[…] Stomach acid is the first line of defense against microbes, but when the stomach pH isn’t low enough, pathogens may grow around the esophageal sphincter and paralyze the muscle, allowing food to relax back up the esophagus (9). […]
[…] Stomach acid is the first line of defense against microbes, but when the stomach pH isn’t low enough, pathogens may grow around the esophageal sphincter and paralyze the muscle, allowing food to relax back up the esophagus (9). […]
[…] https://nutritionreview.org/2013/04/gastric-balance-heartburn-caused-excess-acid/ […]
[…] Gastric Balance. Heartburn Not Always Caused by Excess Acid. Nutrition Reviews April 22, 2013 […]
[…] Stomach acid is the first line of defense against microbes, but when the stomach pH isn’t low enough, pathogens may grow around the esophageal sphincter and paralyze the muscle, allowing food to relax back up the esophagus (9). […]
[…] https://nutritionreview.org/2013/04/gastric-balance-heartburn-caused-excess-acid/ […]
[…] Sources: (1) Takumi K, de Jonge R, Havelaar A. Modeling inactivation of Escherichia coli by low pH: application to passage through the stomach of young and elderly people. J. Appl Microbiol 2000 Dec;89(6):935-43.(2) Wright JV. Treatment of childhood asthma with parenteral vitamin B12, gastric re-acidification, and attention to food allergy, magnesium and pyridoxine. Three case reports with background and an integrated hypothesis. J Nutr Med 1990;1:277-282.https://nutritionreview.org/2013/04/gastric-balance-heartburn-caused-excess-acid/ […]
[…] 许许多多的研究表明,胃酸的分泌随年龄的增加而减少。在一项研究中发现,30%的60岁以上的人群患有萎缩性胃炎,萎缩性胃炎的患者基本不会分泌胃酸。另一项研究发现,40%的80岁以上的女性完全不分泌胃酸。 […]
[…] “Heartburn, a burning sensation in the chest caused by the regurgitation of bile through the stomach into the lower esophagus, is a frequent symptom of low gastric acid. The traditional approach of treating heartburn is to suppress gastric acid by taking antacids or alkalizers. This approach is the opposite of what should often be done, and in many cases only worsens the problem by suppressing gastric acidity when it is needed and promoting it (rebound phenomenon) when it is unnecessary.” https://nutritionreview.org/2013/04/gastric-balance-heartburn-caused-excess-acid/ […]
[…] natural function of our body. Not only that, but many people who are diagnosed with acid reflux may actually have LOW stomach acid, which was the case for […]
[…] http://umm.edu/health/medical/ency/articles/stomach-acid-test https://nutritionreview.org/2013/04/gastric-balance-heartburn-caused-excess-acid/ http://articles.mercola.com/sites/articles/archive/2009/06/02/apple-cider-vinegar-hype.aspx […]
[…] but the underlying problem with heartburn or reflux is too little acid, not too much. As the chart below illustrates, if excessive stomach acid was the problem, we’d see a lot more school children […]
[…] Stomach acid is the first line of protection against microorganisms, yet when the stomach pH isn’t sufficiently low, pathogens may become around the esophageal sphincter and incapacitate the muscle, permitting nourishment to relax back up the esophagus (9). […]
[…] Stomach acid is the first line of defense against microbes, but when the stomach pH isn’t low enough, pathogens may grow around the esophageal sphincter and paralyze the muscle, allowing food to relax back up the esophagus (9). […]
[…] Stomach acid is the first line of defense against microbes, but when the stomach pH isn’t low enough, pathogens may grow around the esophageal sphincter and paralyze the muscle, allowing food to relax back up the esophagus (9). […]
[…] [9] https://nutritionreview.org/2013/04/gastric-balance-heartburn-caused-excess-acid/ [10] http://onlinelibrary.wiley.com/doi/10.1111/1750-3841.12434/full [11] […]
[…] [9] https://nutritionreview.org/2013/04/gastric-balance-heartburn-caused-excess-acid/ [10] http://onlinelibrary.wiley.com/doi/10.1111/1750-3841.12434/full [11] […]
[…] Stomach acid is the first line of protection against microorganisms, yet when the stomach pH isn’t sufficiently low, pathogens may become around the esophageal sphincter and incapacitate the muscle, permitting nourishment to relax back up the esophagus (9). […]
[…] Stomach acid is the first line of protection against microorganisms, yet when the stomach pH isn’t sufficiently low, pathogens may become around the esophageal sphincter and incapacitate the muscle, permitting nourishment to relax back up the esophagus (9). […]
[…] Stomach acid is the first line of protection against microorganisms, yet when the stomach pH isn’t sufficiently low, pathogens may become around the esophageal sphincter and incapacitate the muscle, permitting nourishment to relax back up the esophagus (9). […]
[…] natural function of our body. Not only that, but many people who are diagnosed with acid reflux may actually have LOW stomach acid, which was the case for […]
[…] GASTRIC BALANCE: HEARTBURN NOT ALWAYS CAUSED BY EXCESS ACID […]
[…] Salt also helps with digestion because chloride ions (most people forget that salt consists of sodium and chloride) are secreted in gastric juice as hydrochloric acid, which helps to break down food (6). […]
[…] 7. J Am Geriatr Soc. 1986 Nov;34(11):800-6 8. https://nutritionreview.org/2013/04/gastric-balance-heartburn-caused-excess-acid/ 9. Gut. 1982;23:545-551. 10. Gut. 1969;10:299-302. 11. Unpublished paper: […]
[…] Stomach acid is the first line of protection against microorganisms, yet when the stomach pH isn’t sufficiently low, pathogens may become around the esophageal sphincter and incapacitate the muscle, permitting nourishment to relax back up the esophagus (9). […]
[…] Stomach acid is the first line of protection against microorganisms, yet when the stomach pH isn’t sufficiently low, pathogens may become around the esophageal sphincter and incapacitate the muscle, permitting nourishment to relax back up the esophagus (9). […]
[…] Stomach acid is the first line of defense against microbes, but when the stomach pH isn’t low enough, pathogens may grow around the esophageal sphincter and paralyze the muscle, allowing food to relax back up the esophagus (9). […]
[…] [9] https://nutritionreview.org/2013/04/gastric-balance-heartburn-caused-excess-acid/ [10] http://onlinelibrary.wiley.com/doi/10.1111/1750-3841.12434/full [11] […]
[…] studies (you can geek out some more here) behind this show us that our stomach acidity decreases the older that we get and we can also see […]
[…] Y son estas causas las que pueden favorecer el reflujo ácido (5). […]
[…] 7. J Am Geriatr Soc. 1986 Nov;34(11):800-6 8. https://nutritionreview.org/2013/04/gastric-balance-heartburn-caused-excess-acid/ 9. Gut. 1982;23:545-551. 10. Gut. 1969;10:299-302. 11. Unpublished paper: […]
[…] Gastric Balance: Heartburn Not Always Caused by Excess Acid – NutritonReview.org […]
[…] The older we get, the more alkaline the acid in our stomach becomes. When it comes to our enzyme production, this means the likelihood that the acids triggered by chyme entering our intestine could fail. This is bad because when the acid triggers fail, it starts a chain reaction and secretin isn’t released, which in turn stops pancreatic secretions. In fact, the more we age, the more likely digestive issues can result from enzyme deficiency or low levels of stomach acid. (4) […]
[…] Concurrent illnesses aside, as we age there’s increasing suspicion that digestive problems may result from either low stomach acid or enzyme insufficiency in the elderly, which could be what causes acid reflux. (5) […]
[…] is decreased absorption of vitamins due to gastric imbalances. Jim English wrote in an article for Nutrition Review that our body’s ability to properly digest food and absorb vital nutrients declines with […]
[…] Stomach acid is the first line of defense against microbes, but when the stomach pH isn’t low enough, pathogens may grow around the esophageal sphincter and paralyze the muscle, allowing food to relax back up the esophagus (9). […]
[…] результатам еще одного исследования примерно у 40% женщин старше 80 лет соляная кислота не […]
[…] the esophageal sphincter and paralyze the muscle, allowing food to relax back up the esophagus (9). Taking a Tbs of raw ACV with each meal ensures that the stomach acid will be acidic enough to do […]
[…] sphincter and paralyze the muscle, allowing food to relax back up the esophagus (9). Taking a Tbs of raw ACV with each meal ensures that the stomach acid will be acidic enough to do […]
[…] Stomach acid is the first line of protection against microorganisms, yet when the stomach pH isn’t sufficiently low, pathogens may become around the esophageal sphincter and incapacitate the muscle, permitting nourishment to relax back up the esophagus (9). […]
[…] Stomach acid is the first line of defense against microbes, but when the stomach pH isn’t low enough, pathogens may grow around theesophageal sphincter and paralyze the muscle, allowing food to relax back up the esophagus (9). […]
[…] with meals that include animal protein—you may not be producing enough stomach acid. (6 ) Also known as hypochlorhydria, low stomach acid can make you feel like food is just “sitting” […]
[…] constantly eat an overly alkaline diet, it is relatively easy to demonstrate scientifically that insufficient stomach acid will significantly impair protein digestion and vitamin […]
[…] Stomach acid is the first line of protection against microorganisms, yet when the stomach pH isn’t sufficiently low, pathogens may become around the esophageal sphincter and incapacitate the muscle, permitting nourishment to relax back up the esophagus (9). […]
[…] Naturopathy has for long been successfully prescribing Betaine hydrochloride (HCl) a nutritional supplement to restore gastric acidity and to support healthy gut function. You can […]
[…] https://nutritionreview.org/2018/03/gastric-balance-heartburn-caused-excess-acid/ […]
[…] like chronic gastritis or gastric carcinoma, pernicious anemia, pellagra, and alcoholism. (4) Signs that you’re likely not making enough gastric juices include lack of appetite, fullness […]
[…] like chronic gastritis or gastric carcinoma, pernicious anemia, pellagra, and alcoholism. (4) Signs that you’re likely not making enough gastric juices include lack of appetite, fullness […]