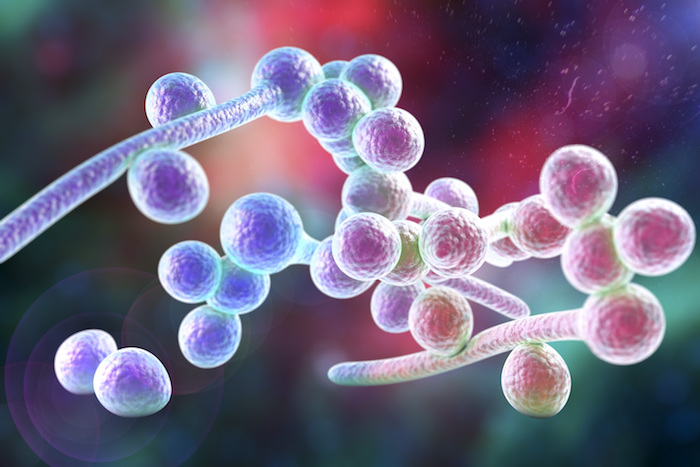
 Scientists have discovered how a common yeast, Candida albicans, adapts to low oxygen levels in different parts of the body, allowing it to emerge to cause infection and harm its host. Candida is a natural part of the human microflora – the vast community of natural microorganisms that commonly live in our bodies. Most often found in the GI tract, the mouth and vagina, C. albicans is the most common cause of genital yeast infections, urinary tract infections (UTIs) and oral thrush.
Scientists have discovered how a common yeast, Candida albicans, adapts to low oxygen levels in different parts of the body, allowing it to emerge to cause infection and harm its host. Candida is a natural part of the human microflora – the vast community of natural microorganisms that commonly live in our bodies. Most often found in the GI tract, the mouth and vagina, C. albicans is the most common cause of genital yeast infections, urinary tract infections (UTIs) and oral thrush.
Candida is usually held in check by a healthy immune system, but when our natural immune barrier fails – due to use of antibiotics, immunosuppressive diseases or diabetes – C. albicans turns into an opportunistic pathogen, emerging from hidden reservoirs to spread throughout the body and trigger life-threatening, systemic diseases.
Systemic infection, which often results in sepsis, takes the lives of the vast majority of critically-ill patients in a rapid manner and is considered a global threat. According to the World Health Organization, sepsis is estimated to affect more than 30 million people worldwide every year, potentially leading to 6 million deaths. From those 3 million are newborns and 1.2 million are children.
Candida albicans is the most common fungal pathogen and a common cause of sepsis. While most people are infected with Candida albicans since birth, the infection causes serious illness or even death, particularly among those with a weakened immune system.
The current study is a step towards characterizing the body’s immune responses under low oxygen levels, a frequent stress condition during inflammation and infection. Neutrophils, the most abundant white blood cell and essential defense line against fungal microbes, were shown to be particularly hampered in their ability to attack and eradicate C. albicans under low oxygen conditions.
Studying C. albicans adaption to low oxygen niches is particularly useful, since it helps researchers understand the pathogenicity of the yeast and can and development of better therapies.
“It was very surprising to see that the fungus does not require oxygen to cause disease. Unexpectedly, the microbial pathogen could even use low oxygen environments to evade immune attack and to become more virulent,” says Constantin Urban, Associated Professor at the Department of Clinical Microbiology at Umeå university.
The recent work of his group aims to better understand how adaption of microbial fungi to low oxygen environments influences their recognition by immune cells and their ability to thrive and cause harmful infection within the host.
“We now understand how C. albicans, under these circumstances, exploits the training from anoxic commensal niches to thrive in deep-seeded body sites which quickly induce inflammation and immune cell recruitment. Both processes rapidly exhaust oxygen and in turn create low oxygen milieus.”
“Our work is clinically relevant, since current fungal therapy is hampered by toxic side effects and ineffectiveness. We gained insight into mechanisms which fungal pathogens use to circumvent immune surveillance in environments lacking oxygen. Hence, our study aims for identification of future therapy strategies to reduce premature deaths and to improve patients’ life quality. But I always liked to think outside the box,” explains Pedro Lopes, recently graduated PhD student in the group and first author of the study.
“Fungi are very versatile organisms which can grow at almost any place. Interestingly, growing fungi were spotted at the international space station (ISS).”
“Ongoing research attempts to elucidate how fungal microbes thrive under these conditions. Our investigations open up new avenues to study fungal adaptation to hypoxic environments, such as within our bodies or at space stations.”
Source: José Pedro Lopes, Marios Stylianou, Emelie Backman, Sandra Holmberg, Jana Jass, Rolf Claesson, Constantin F. Urban. Evasion of Immune Surveillance in Low Oxygen Environments Enhances Candida albicans Virulence. mBio, 2018; 9 (6) DOI: 10.1128/mBio.02120-18











