 New research suggests that the common dietary supplement, choline, may play a role in preventing Alzheimer’s disease (AD). Closely related to the B complex family of vitamins, choline is found in virtually all living cells where it plays a role in manufacturing cellular membranes. In the brain choline is converted into acetylcholine, a vital neurotransmitter responsible for memory, muscle control and mood. Choline also is used to direct metabolic functions and plays a vital role in regulating gene expression. Choline is also needed for the production and metabolization of fats and cholesterol, and aids in protecting the liver from the accumulation of excess fatty deposits.
New research suggests that the common dietary supplement, choline, may play a role in preventing Alzheimer’s disease (AD). Closely related to the B complex family of vitamins, choline is found in virtually all living cells where it plays a role in manufacturing cellular membranes. In the brain choline is converted into acetylcholine, a vital neurotransmitter responsible for memory, muscle control and mood. Choline also is used to direct metabolic functions and plays a vital role in regulating gene expression. Choline is also needed for the production and metabolization of fats and cholesterol, and aids in protecting the liver from the accumulation of excess fatty deposits.
The primary dietary sources of choline include beef, eggs, dairy products, fish, and chicken, with lower levels found in nuts, beans, and cruciferous vegetables such as broccoli. Choline is also produced by the human liver, but not in the amounts needed to meet the body’s requirements. Choline is also available as an inexpensive and safe dietary supplement.
Choline and Alzheimer’s Disease
It is well understood that Alzheimer’s disease causes harm to the brain long before clinical symptoms are evident. And once symptoms appear, it’s too late – the disease is currently irreversible. In addition to disorientation and impaired memory function, Alzheimer’s causes loss of motor control in those who are afflicted.
Approximately 6 million individuals are living with Alzheimer’s in the U.S., and deaths from the disease are increasing, rising by a stunning 89 percent between 2000 and 2014. Alzheimer’s is now projected to afflict 14 million Americans over the next four decades, with costs for managing the disease expected to exceed $20 trillion. Most worrisome to experts is the fact that 75 percent of those with Alzheimer’s have yet to be diagnosed. To develop more effective treatments researchers are racing to understand the disease itself.
One of the most disturbing findings to date is that women are at a particularly increased risk of developing Alzheimer’s disease.
Women and Alzheimer’s
In their new study, researchers at the Banner Neurodegenerative Disease Research Center (NDRC) examined choline’s potential role in alleviating the effects of Alzheimer’s disease. Since two-thirds of those afflicted with Alzheimer’s disease are women the researchers worked with female mice that were specially bred to develop AD-like symptoms. In a previous study they determined that feeding choline to pregnant mice helped to protect the offspring, preventing their babies from developing Alzheimer’s as they matured. Building on that prior research they designed their new study to evaluate the benefits of giving choline to adult female mice also bred to develop Alzheimer’s.
Their results showed that female mice fed on a high-choline diet throughout life showed improvements in spatial memory, compared with those receiving less choline.
These findings were supported by another early study that demonstrated benefits of lifelong choline supplementation in male mice with AD-like symptoms. “Our results nicely replicate findings by this group in females,” Velazquez says.
Brain Eliminate Harmful Debris
Their research revealed how choline supplementation protects the brain from Alzheimer’s disease in two ways. First, choline blocks the production of amyloid-beta plaques, the hallmark of Alzheimer’s disease. Mice supplemented with choline were found to have reduced levels of toxic amyloid-beta formations in their hippocampus, a brain region known to play a central role in memory formation.
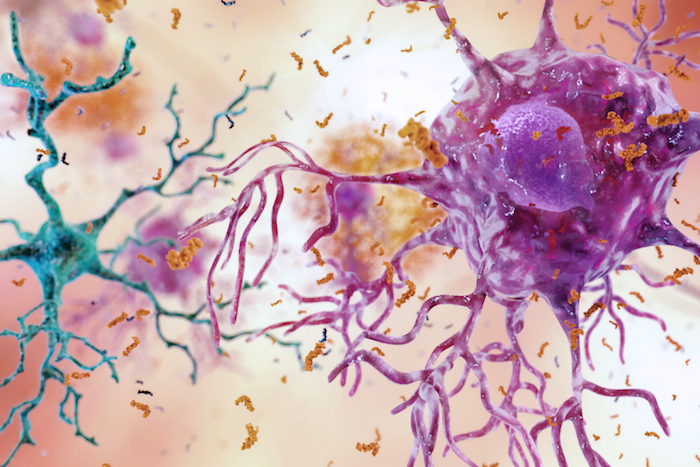
Secondly, choline supplementation was shown to reduce the activation of microglia, a type of specialized cell that helps the brain rid itself of harmful debris.
Microglia normally help to keep the brain healthy, but over-active microglia have been shown to trigger brain inflammation and neuronal death, both common symptoms of AD. “We found that lifelong choline supplementation altered the alpha7 nicotinic acetylcholine and Sigma-1 receptor,” resulting in the reduction of diseased associated activated microglia and improvements in behavior, Velazquez said.
The observed reductions in disease-associated microglia, which are observed in numerous other neurodegenerative diseases, points the way to potential new treatments for a broad range of issues, including traumatic brain injuries, multiple sclerosis and Parkinson’s disease.
Human Choline Deficiency
Another recently published paper in the British Medical Journal (BMJ) raises concerns over the current trend toward plant-based diets, warning that an unintended deficiency in dietary choline intake may also be placing unborn children at risk. “Choline is transported to the fetus in utero. It’s an important nutrient because it’s involved in the development of the brain and spinal cord. Shortfalls could impact the cognitive development of children after they’re born,” according to Emma Derbyshire BSc, PhD, RNutr, and author of the paper.
Derbyshire says choline should be of particular concern for those eating fewer animal products. There are plant sources of choline, such as nuts and soya beans, but they contain far less than eggs and red meat (see graph below). “You can get it, but you have got to be very rigorous in your diet,” says Derbyshire.
|
|
The biggest concern over choline intake is connected to fetal brains. As mentioned in the NDRC study, choline is needed to build brains, and when pregnant mice are deprived of choline their babies do worse at mental tasks, like negotiating mazes.
There have been a few small trials to see if giving pregnant women higher doses of choline helps their fetuses’ brain development. Results are mixed, but one of the longest trials showed that when the women took twice the recommended dose of choline while pregnant, their children did better at a simple memory task when 7 years old.
“There’s something very special about this nutrient,” says Marie Caudill at Cornell University in New York, who helped run the trial.
And choline does more just affect the brain while it is developing. As the previous study in mice suggests, higher choline intake in adulthood staves off the effects of dementia.
For babies and fetuses at least, there is growing consensus that choline is essential. Baby milk manufacturers must now ensure a minimum level in their products, both in the US and Europe. And in 2018, the American Academy of Pediatrics called for pregnant women to ensure they are getting enough choline.
Revising Adult Choline Intake Guidelines
It is still unclear exactly how much choline we need. But because eggs and red meat are some of the best sources of choline, the trend for eating fewer animal products could mean we are missing out on this vital nutrient without knowing it. Even those of us who eat meat might not be getting enough.
Unusual Path to Uncovering Choline’s Vital Role in Human HealthIn the past, most vitamins were discovered because people who were malnourished got a characteristic disease that was cured when they ate certain foods. Sailors deprived of fresh fruit got scurvy because they lacked vitamin C, for example. Choline’s history is less straightforward. It was first isolated from bile in 1862 and was later found to play many roles in the human body, from controlling liver fat metabolism to making the nerve signaling molecule, acetylcholine. At the time it was thought that the human body could make its own choline, since it produces plenty of other biochemicals, and there was no known choline deficiency disease. This assumption was overturned in the 1980s when studies revealed that some animals get sick on a diet lacking in choline. Steven Zeisel at the University of North Carolina then devised a definitive test by getting volunteers to stay in hospital for several weeks eating only the food provided. His team created a baseline diet with very little choline – mainly salads, a soy-based protein shake and bread rolls. Some people got rolls with added choline, some didn’t. Within a few weeks, the volunteers who got rolls without choline had more liver enzymes in their blood and their livers accumulated fat. When they were switched onto the choline-laced bread, they recovered. “I had discovered the first new nutrient since the basic vitamins,” says Zeisel. Because of this and other lines of research, choline was reassessed. It turned out that human breast milk is rich in choline, and that pregnant women pump it across their placenta. Levels can be 10 times higher in fetuses than in mothers’ blood. That had to be for a reason. |
It is now accepted that adult livers can make some choline, but most of us don’t produce enough to meet our daily requirements. In 1998, the US Institute of Medicine advised that men should consume 550 milligrams a day and women 425 mg (more if they are pregnant or breastfeeding).
Still, some people may need more choline than others. About one in three people in the US have a mild case of fatty liver. This is usually blamed on unhealthy eating. But Zeisel says lack of choline may be responsible in some cases. He has shown that people with fatty liver are more likely to have certain gene variants that mean they make less choline.
Revising Choline Intake Guidelines
The current established adequate intake level of choline for adult women is 425mg/day, and 550mg/day for adult men. Growing evidence indicates that even this current recommended daily intake (RDI) may not be optimal for healthy aging, especially in women. This is relevant, given the higher incidence of Alzheimer’s disease in women.
This suggests that additional choline in diet may be beneficial in preventing neuropathological changes associated with the aging brain.
The Tolerable Upper Limit (TUL) of choline that is unlikely to cause side effects for adult females and males is 3,500mg/day, which is 8.24 times higher than the current recommendation for females and 6.36 times higher than the current recommendation for males.
Choline can be found in various foods. According to the USDA, high levels of choline are found in chicken liver (3oz; 247mg), eggs (1 large egg with yolk;147mg), beef grass-fed steak (3oz; 55mg), wheat germ (1oz toast; 51mg), milk (8oz; 38mg), and Brussels sprouts (1/2 cup; 32mg). Additionally, vitamin supplements containing choline, for example choline bitartrate and choline chloride, are widely available at affordable costs. The vitamin supplements containing choline are particularly relevant for those who are on plant-based diets.
Summary
Prior research concerning Alzheimer’s has indicated that there is no one factor at play. Rather, a multitude of factors that are believed to contribute to the development of the disease, including genetics, age and lifestyle. Additionally, research suggests that diet can have a significant effect in increasing or lowering the risk of cognitive decline.
These studies show that simply adding choline to the diet throughout life can benefit fetal development and may reduce Alzheimer’s pathology in those most affected by the disease.
Additionally, these results have implications for other neurodegenerative afflictions where activated microglia are rampant.
Choline is considered a very safe alternative, compared with many pharmaceuticals. “At 4.5 times the RDI (recommended daily intake), we are well under the tolerable upper limit, making this a safe preventive therapeutic strategy.”
Source: Ramon Velazquez, Eric Ferreira, Sara Knowles, Chaya Fux, Alexis Rodin, Wendy Winslow, Salvatore Oddo. Lifelong choline supplementation ameliorates Alzheimer’s disease pathology and associated cognitive deficits by attenuating microglia activation. Aging Cell, 2019; DOI: 10.1111/acel.13037.













Some practitioners, Dr Dale Bredesen for one, are reporting a reversal in Alzheimers in some of they patients on protocol.
[…] Source […]