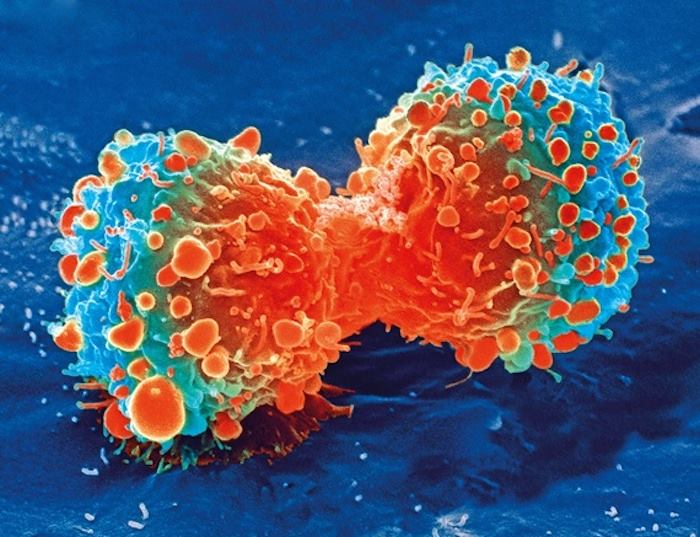
 In a finding that could herald a major breakthrough in cancer treatment British scientists have accidentally discovered a new type of immune cell that kills most types of cancers.
In a finding that could herald a major breakthrough in cancer treatment British scientists have accidentally discovered a new type of immune cell that kills most types of cancers.
Researchers at Cardiff University were analyzing blood samples from a blood bank in Wales, looking for immune cells that could fight bacteria, when they found an entirely new type of T-cell.
That new immune cell carries a never-before-seen receptor which acts like a grappling hook, latching on to most human cancers, while ignoring healthy cells.
In laboratory studies, immune cells equipped with the new receptor were shown to kill lung, skin, blood, colon, breast, bone, prostate, ovarian, kidney and cervical cancer.
Professor Andrew Sewell, lead author on the study and an expert in T-cells from Cardiff University’s School of Medicine, said it was “highly unusual” to find a cell that had broad cancer-fighting therapies, and raised the prospect of a universal therapy.
“This was a serendipitous finding, nobody knew this cell existed,” Prof Sewell told The Telegraph.
“Our finding raises the prospect of a ‘one-size-fits-all’ cancer treatment, a single type of T-cell that could be capable of destroying many different types of cancers across the population. Previously nobody believed this could be possible.”
Asked if it meant that someone in Wales was walking around completely immune to cancer, Prof Sewell said: “Possibly. This immune cell could be quite rare, or it could be that lots of people have this receptor but for some reason it is not activated. We just don’t know yet.”
Therapies which engineer immune cells to fight specific types of cancer already exist, but they are currently only useful for some forms of leukaemia, and do not work for solid tumours, which account for most cancers.
Those treatments – known as CAR-T and TCR-T therapies – involve taking immune cells from a patient which are then altered so they can lock onto molecules which sit on the surface of cancer cells.
The cells are then grown in huge numbers and injected back into the patient’s bloodstream.
CAR-T therapy is now given for certain forms of leukaemia but does not work for solid tumours, the vast majority of cancers. TCR-T therapies can work in some other cancers but they need to lock onto molecules called HLA, which vary widely in the population.
In contrast, the new cell attaches to a molecule on cancer cells called MR1, which does not vary in humans.
It means that not only would the treatment work for most cancers, but it could be shared between people, raising the possibility that banks of the special immune cells could be created for instant ‘off-the-shelf’ treatment in future.
When researchers injected the new immune cells into mice bearing human cancer and with a human immune system, they found ‘encouraging’ cancer-clearing results.
And they showed that T-cells of skin cancer patients, which were modified to express the new receptor, could destroy not only the patient’s own cancer cells, but also other patients’ cancer cells in the laboratory.
Prof Sewell said the ‘right people’ are now interested in developing the potential new therapy and said progress could now move ‘quite fast’. The team says human trials on terminally ill patients could begin as early as November if the new treatment passes further laboratory safety testing.
Professor Oliver Ottmann, Cardiff University’s Head of Haematology, whose department delivers CAR-T therapy, said: “This new type of T-cell therapy has enormous potential to overcome current limitations of CAR-T, which has been struggling to identify suitable and safe targets for more than a few cancer types.”
Professor Awen Gallimore, of the University’s division of infection and immunity and cancer immunology lead for the Wales Cancer Research Centre, added: “If this transformative new finding holds up, it will lay the foundation for a ‘universal’ T-cell medicine, mitigating against the tremendous costs associated with the identification, generation and manufacture of personalised T-cells.
“This is truly exciting and potentially a great step forward for the accessibility of cancer immunotherapy.”
Commenting on the study, Daniel Davis, Professor of Immunology at the University of Manchester, said it was an exciting discovery which opened the door to cellular therapies being used for more people.
“We are in the midst of a medical revolution harnessing the power of the immune system to tackle cancer. But not everyone responds to the current therapies and there can be harmful side-effects.
“The team have convincingly shown that, in a lab dish, this type of immune cell reacts against a range of different cancer cells.
“We still need to understand exactly how it recognises and kills cancer cells, while not responding to normal healthy cells.”
The research was published in the journal Nature Immunology.











