 A new cartilage-like material could make the job of repairing damaged knees much easier. The thin, slippery layer of cartilage cushioning the bones in your knee is magical stuff: strong enough to withstand your weight, yet soft and supple enough to absorb heavy loads and impacts over decades of repeated use. This combination of soft-yet-strong has been hard to reproduce in the lab, but now researchers from Duke University have developed an novel hydrogel — a material made of water-absorbing polymers — that matches the strength and durability of human cartilage.
A new cartilage-like material could make the job of repairing damaged knees much easier. The thin, slippery layer of cartilage cushioning the bones in your knee is magical stuff: strong enough to withstand your weight, yet soft and supple enough to absorb heavy loads and impacts over decades of repeated use. This combination of soft-yet-strong has been hard to reproduce in the lab, but now researchers from Duke University have developed an novel hydrogel — a material made of water-absorbing polymers — that matches the strength and durability of human cartilage.
The researchers are developing the compound to serve as a replacement for damaged joint cartilage, and to reduce the need for the 600,000 knee replacement surgeries performed in the U.S. each year.
Replacing Damaged Cartilage
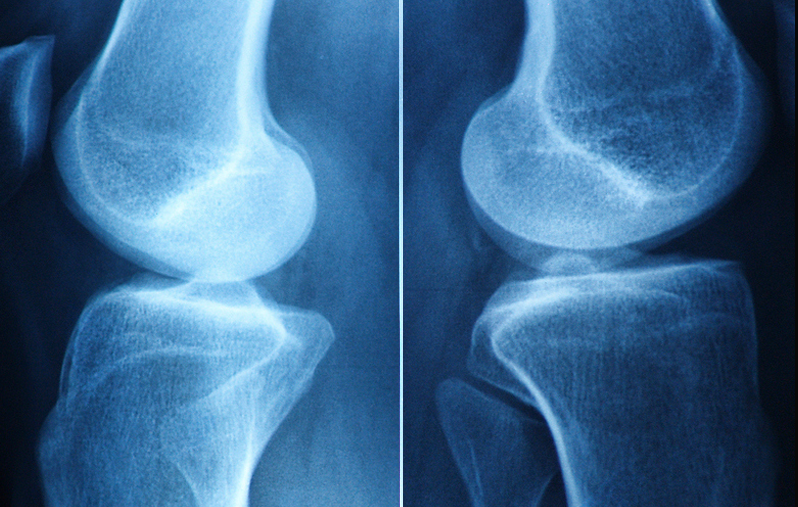
Cartilage is a smooth rubbery tissue that covers the ends of bones and enables them to glide smoothly against each other, helping to absorb a huge amount of force with every step – typically between two and three times your body weight.
However, cartilage also has limited ability to heal and repair itself. Once worn by age, overuse or trauma it’s difficult to treat.
For people seeking to avoid or postpone a knee replacement (that may only last for 20 years), artificial cartilage can help. Hydrogels have been explored for use as a cartilage substitute since the 1970s and are used in soft contact lenses and disposable diapers. Researchers are attracted to these materials because of their slippery, shock-absorbing properties and because they don’t harm nearby cells. But until now they’ve proven too weak to be used in load-bearing joints like the knee.
The new hydrogel consists of two intertwined polymer networks: one made of stretchy spaghetti-like strands and the other more rigid and basketlike, with negative charges along their length. These are reinforced with a third ingredient, a meshwork of cellulose fibers.
When the gel is stretched, the cellulose fibers resist pulling and help hold the material together. And when it is squeezed, the negative charges along the rigid polymer chains repel each other and stick to water, helping it spring back to its original shape.
Despite being 60% water, a single quarter-sized disc of the new hydrogel is incredibly strong.
When the researchers compared the resulting material to other hydrogels, theirs was the only one that was as strong as cartilage under both squishing and stretching.
In one experiment, the team subjected it to 100,000 cycles of repeat pulling, and the material held up just as well as porous titanium used for bone implants, “which exceeded our initial expectations,” said co-author William Koshut, a PhD student in the Gall lab.
They also rubbed the new material against natural cartilage a million times. They found that its smooth, slippery self-lubricating surface is as wear-resistant as the real thing and four times more wear-resistant than synthetic cartilage implants currently FDA-approved for use in the big toe.
“Only this combination of all three components is both flexible and stiff and therefore strong,” said co-author Feichen Yang.
In addition to developing the new artificial cartilage, researchers at Duke have been working with 3D printers to make replacement parts that are an exact fit for each individual knee. Their work has shown that hydrogel replacement parts can be produced by a 3D “bio-printer” in a single day, and for as little as $300 each.
Moving the material from the lab to the clinic would take another three years at least, but the team says eventually the research could offer new options for people with knee pain, and get them back to doing the things they love without the long recovery times and limited lifetime associated with cartilage repair or knee replacement surgery.
Source: Feichen Yang, Jiacheng Zhao, William J. Koshut, John Watt, Jonathan C. Riboh, Ken Gall, Benjamin J. Wiley. A Synthetic Hydrogel Composite with the Mechanical Behavior and Durability of Cartilage. Advanced Functional Materials, 2020; 2003451 DOI: 10.1002/adfm.202003451











