Brain tumors fly under the radar of the body’s defense forces by coating their cells with extra amounts of a specific protein, new research shows. Like a stealth fighter jet, the coating means the cells evade detection by the early-warning immune system that should detect and kill them. The stealth approach lets the tumors hide until it’s too late for the body to defeat them.
The findings, made in mice and rats, show the key role of a protein called galectin-1 in some of the most dangerous brain tumors, called high grade malignant gliomas. A research team from the University of Michigan Medical School made the discovery and has published it online in the journal Cancer Research.
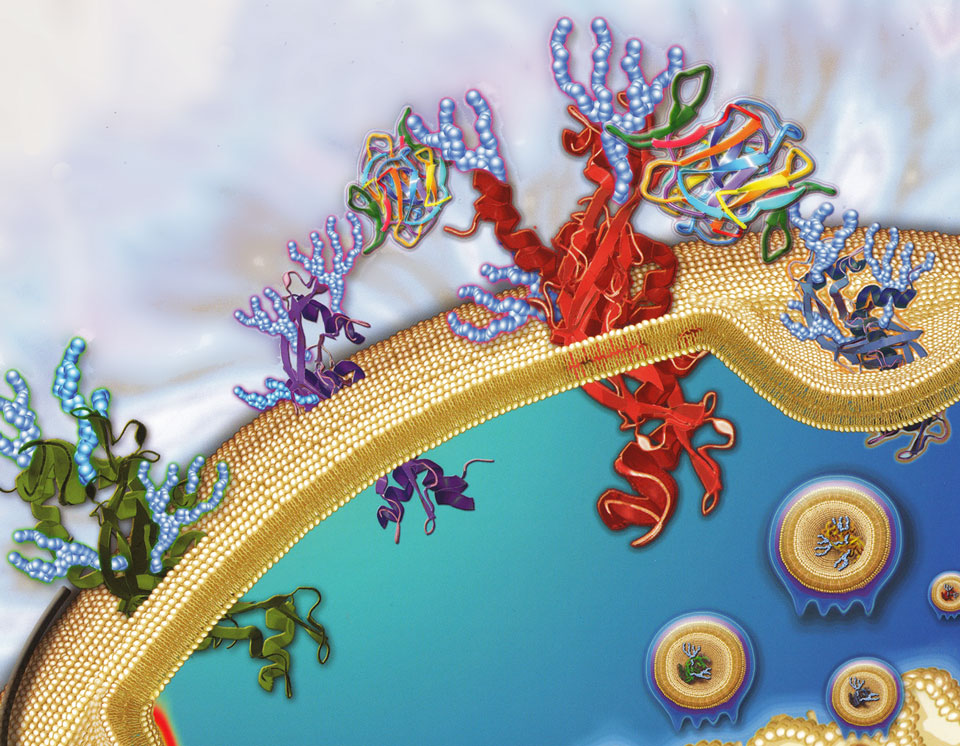
Image: Golgi production of branched N-glycans on surface glycoproteins
leading to enhanced binding of extracellular galectin-3.
In a stunning example of scientific serendipity, the team uncovered galectin-1’s role by pursuing a chance finding. They had actually been trying to study how the extra production of galectin-1 by tumor cells affects cancer’s ability to grow and spread in the brain.
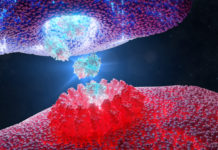
Instead, they found that when they blocked cancer cells from making galectin-1, the tumors were eradicated; they did not grow at all. That’s because the “first responders” of the body’s immune system – called natural killer or NK cells – spotted the tumor cells almost immediately and killed them.
But when the tumor cells made their usual amounts of galectin-1, the immune cells couldn’t recognize the cancerous cells as dangerous. That meant that the immune system couldn’t trigger the body’s “second line of defense”, called T cells – until the tumors had grown too large for the body to beat.
Team leader Pedro Lowenstein, M.D., Ph.D, of the U-M Department of Neurosurgery, says the findings open the door to research on the effect of blocking galectin-1 in patients with gliomas.
“This is an incredibly novel and exciting development, and shows that in science we must always be open-minded and go where the science takes us; no matter where we thought we wanted to go,” says Lowenstein, whose graduate student Gregory J. Baker is the first author of the paper.
“In this case, we found that over-expression of galectin-1 inhibits the innate immune system, and this allows the tumor to grow enough to evade any possible effective T cell response,” he explains. “By the time it’s detected, the battle is already lost.”
The NK-evading “stealth” function of the extra-thick coating of galectin-1 came as a surprise, because glioma researchers everywhere had assumed the extra protein had more to do with the insidious ability of gliomas to invade the brain, and to evade the attacks of T cells.
Gliomas, which make up about 80 percent of all malignant brain tumors, include anaplastic oligodendrogliomas, anaplastic astrocytomas, and glioblastoma multiforme. More than 24,000 people in the U.S. are diagnosed with a primary malignant brain tumor each year.
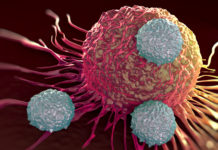
The tiny tendrils of tumor that extend into brain tissue from a glioma are what make them so dangerous. Even when a neurosurgeon removes the bulk of the tumor, small invasive areas escape detection and keep growing, unchecked by the body.
Helping the innate immune system to recognize early stages of cancer growth, and sound the alarm for the body’s defense system to act while the remaining cancer is still small enough for them to kill, could potentially help patients.
While the new discovery opens the door to that kind of approach, much work needs to be done before the mouse-based research could help human patients, says Lowenstein, who is the Richard Schneider Collegiate Professor in Neurosurgery and also holds an appointment in the U-M Department of Cell and Developmental Biology. Galectin-1 may help other types of tumor evade the innate NK cells, too
The new research suggests that in the brain’s unique environment, galectin-1 creates an immunosuppressive effect immediately around tumor cells. The brain cancer cells seem to have evolved the ability to express their galectin-1 genes far more than normal, to allow the tumor to keep growing.
Lowenstein and co-team leader Maria Castro, Ph.D., have long studied the immune system’s interactions with brain cancer, using funding from the National Institutes of Health, and are co-leading a new clinical trial for malignant glioma (NCT01811992), that aims to translate prior research achievements into new trials for patients with brain tumors.
Most brain tumor immune research has focused on triggering the action of the adaptive immune system – whose cells control the process that allows the body to kill invaders from outside or within.
But that system take days or even weeks to reach full force – enough time for incipient tumors to grow too large for immune cells to eliminate solid tumor growth. The new research suggests the importance of enhancing the ability of the innate immune system’s “early warning” sentinels to spot glioma cells as early as possible.
Source: Cancer Research, OnlineFirst, doi:10.1158/0008-5472.CAN-14-1203,http://cancerres.aacrjournals.org/content/early/2014/07/18/0008-5472.CAN-14-1203.abstract