Restoring Thymic Function for Immune Support and Life Extension
By Ward Dean, MD and Jim English
The key to a healthy, functioning immune system rests largely with the thymus gland, a small organ lying just beneath the breast- bone (Fig. 1). Weighing less than half of an ounce at birth, by puberty, the thymus will grow to its maximum size of about 10 ounces. After age 20, the thymus begins to shrink (atrophy) and thymic cells progressively die off to be replaced by fat and connective tissue. (1)
This age-related atrophy of the thymus gland – and the subsequent decline of thymic hormones – gradually robs the body of its ability to fight off infectious diseases, autoimmune diseases, and cancer. As immunologist Keith Kelly noted: “The involution [shrinkage] of the thymus gland is one of the cardinal bio-markers of aging.” (2)
Thymus and Immunity
As discussed previously in the Neuroendocrine Theory of Aging, (Part IV, The Immune Homeostat) the thymus gland interacts with the rest of the endocrine system (the Hypothalamus-Pituitary-Thymus axis) to maintain a healthy immune system. (3) The primary role of the thymus is to assist in the proliferation and differentiation of mature T-lymphocytes — cells that attack and kill viruses and bacteria.
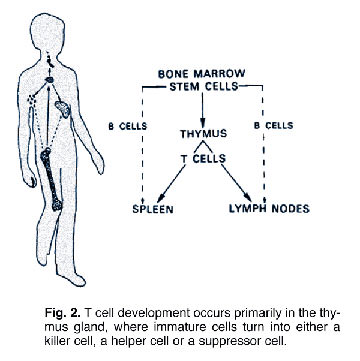
T-lymphocytes (T-cells) and B-lymphocytes (B-cells) are both white blood cells that are produced in bone marrow. B-cells emerge from bone marrow fully mature and ready to go about the business of recognizing invaders (antigens) and signaling the production of antibodies. By contrast, T-cells emerge from marrow in an incomplete state. Before they can begin to function properly, the “immature” T-cells must first migrate to the thymus gland (Fig. 2.) where they “incubate” and are programmed to transform into one of three types of specialized T-cells:
- T-4 Helper Cells. T-4 Helper cells work to orchestrate the immune response by activating other immune cells and stimulating the production of antibodies by the B-cells.
- T-8 Cytotoxic (Killer) Cells. T-8 Killer cells are directed by the T-4 Helper cells to attack and destroy invading viruses and cancer cells.
- T-8 Suppressor Cells. The T-8 Suppressor cells suppress killer cells by signaling the termination of an attack.
Age-Related Decline of Thymic Function
In our early twenties we have an abundance of well-functioning T-cells that regulate the immune system and help the body fight off pathogens and disease. But with the inexorable shrinking of the thymus gland over time, by about age forty the output of thymic hormones has decreased significantly and the T-cells have begun to lose their effectiveness. It is this gradual loss of functioning T-cells that is thought to be responsible for many of the age-related changes in the immune system.Restoring Thymic Function
A number of animal extracts and synthetic thymic hormones have demonstrated the ability to dramatically reverse thymic atrophy and restore levels of immunity to much more youthful levels. In addition to being among the most effective immune-enhancing agents known, thymic extracts and thymic hormones are among the few agents that are documented to extend the life span of experimental animals. (4,5) Many processed thymus extracts generally consists of ground up thymus glands. These products contain a conglomeration of biologically inactive thymus tissues, cell debris, fragments of thymus proteins and thymus by-products.
Thymic Protein A
Terry Beardsley, Ph.D., is an immunologist and experimental biologist from Baylor College of Medicine in Texas. He has been the principal scientist in the Monoclonal Antibody Facility at Smith Kline Beckman; Assistant Professor of research at the University of California at San Diego; Research Associate at Scripps Clinic, La Jolla; and Assistant Research Professor at UCLA’s Laboratory of Nuclear Medicine.
Dr. Beardsley has spent most of his career researching the thymus gland, and is considered one of the leading experts in the world on this subject. In the early 1980s, Dr. Beardsley established the first continuously growing line of thymic stromal cells (cells producing immune-regulating substances such as IL-2) in his laboratory. (6) Dr. Beardsley also succeeded in proving that his cultures possessed higher levels of immune stimulatory activity than seen in previously known cultures. However, his results were less effective than he desired due to the presence of unwanted competing biological activities. (7)
Dr. Beardsley spent the next eight years working tediously with one cell at a time until he isolated a single purified protein that produced all of the immune activity of the mixed thymic cultures – without the presence of any of the other cell types. What Dr. Beardsley had discovered was a complete, biologically “intact” 500-amino chain protein that fits into the receptor sites on T-4 cells to “turn on” and program the cells for their disease-fighting functions. Dr. Beardsley named the peptide Thymic Protein A (TPA).
Following several favorable clinical studies involving both animal (Feline AIDS and distemper) and human (chronic fatigue syndrome [CFIDS] and Epstein-Barr [EBV]) subjects, Dr. Beardsley developed a unique oral delivery system for his formulation which avoided the degradation of the thymic protein in the stomach – a significant problem with other over-the-counter oral thymic preparations.
The scientific data gathered from these studies resulted in the awarding of a US patent to Dr. Beardsley in 1997 for both the Thymic protein A molecule and its method of production.
Safety Issues
In the five-and-a-half years since Thymic Protein A was introduced as an oral nutritional supplement, thousands of individuals have consumed this product. Hundreds of medical doctors are using it for a variety of immune-related illnesses with no adverse reactions from this highly purified, extremely safe, low-dose protein molecule. Thymic Protein A is produced at only one site in the world, under the personal control and supervision of Dr. Beardsley. Based on his commitment to maintaining the highest scientific standards, utmost purity is assured.
Summary
The immune system is clearly an integral component of the neuroendocrine system, which exhibits typical age-related decrements. Previous research with a number of nutritional and/or pharmacological substances has proven that aspects of impaired immune function can be restored to more youthful, healthy levels. Fabris noted that, “age-related thymic involution is not an irreversible process …functional recovery can be achieved even in old age…[and] thymus regrowth can be induced in old age.” (8)
Thymic Protein A has been demonstrated to have immune-enhancing properties. A dose of a mere 4 micrograms of Thymic Protein A may make a major difference in strengthening the immune system through its T-cell “programming” role. The more T-cells that are functioning properly, the greater the immune response against infections and pathogenic agents. The reported benefits of Thymic Protein A include increased stamina, energy, well-being and ability to ward off infections.
Dr. Julian Whitaker states that Thymic protein A “is likely the most powerful natural stimulant of the immune system ever discovered.” (9) Many other physicians such as Drs. Robert Atkins, Abram Ber, Jonathan Wright, Lee Cowden and Serefina Corsello, are using it regularly in their practices and for themselves. Dr. Whitaker recommends one to three packets a day, taken sublingually when sick (I have known cancer patients and very debilitated patients who took six packets daily. WD). Dr. Whitaker also recommends that a maintenance dosage be taken on a daily basis to support age-impaired immune systems. Thymic Protein A is extremely safe, with no adverse effects noted in any dose.
References
1. South, James, “Thymus Gland, Its Overlooked But Vital Role,” Vitamin Research News, November 1999, Vol. 13:11, pp 1-5.
2. K. Kelly et al. “A pituitary-Thymus Connection During Aging.” Ann. N.Y. Acad. Sci. 521, 88-98, 1988.
3. Dean, Ward, MD. “The Neuroendocrine Theory of Aging Part IV – The Immune Homeostat.” Vitamin Research News, October 1999, Vol. 13:10, pp 1-11.
4. Fabris, N., Mocchegiani, E., Muzzioli, M., and Provinciali, M. Neuroendocrine-thymus interactions: Perspectives for intervention in aging. In: Neuroimmunomodulation: Interventions in Aging and Cancer, Ann NY Acad Sci, Vol 621, by Pierpaoli, W. and Spector, N.H., (eds). NY Acad Sci, New York, 1988, 72-87.
5. Cardarelli, Nate. The role of a thymus-pineal axis in an immune mechanism of aging. J Theor Biol, 1990, 145: 397-405.
6. Beardsley TR, Pierschbacher M, Wetzel GD, Hays EF. Induction of T-cell maturation by a cloned line of thymic epithelium (TEPI). Proc Natl Acad Sci USA 1983 Oct;80(19):6005-9.
7. Hays EF, Beardsley TR. Immunologic effects of human thymic stromal grafts and cell lines. Clin Immunol Immunopathol 1984 Dec;33(3):381-90.
8. Fabris, N., Mocchegiani, E., Muzzioli, M., and Provinciali, M. Role of zinc in neuroendocrine-immune interactions during aging. In: Physiological Senescence and Its Postponement, Ann New York Acad Sci, Vol 621, by Walter Pierpaoli and Nicola Fabris, (eds.),1991, NY Acad Sci, New York, 314-326.
9. Whitaker, Julian. Give your immune cells a natural ‘shot in the arm.’ Dr. Julian Whitaker’s Health & Healing, March, 1997, Vol 7, No. 3, 1-2.












[…] NUTRITION REVIEW BY DR. WARD DEAN […]
[…] Thymic Protein A (TPA) […]
[…] Thymic Protein A (TPA) […]
Thymic Protein A is the patented active ingredient in ProBoost. You can learn more about Thymic Protein A and the ProBoost family of products on https://proboostnow.com/