 Getting adequate sleep is key to good health, and studies have shown that insufficient sleep increases the risk of serious problems, including cardiovascular disease. Now Massachusetts General Hospital (MGH) investigators have discovered one way that sleep protects against the buildup of arterial plaques called atherosclerosis. In their paper published in Nature, the researchers describe the mechanism by which insufficient sleep increases production of inflammatory white blood cells known to be major contributors to atherosclerosis.
Getting adequate sleep is key to good health, and studies have shown that insufficient sleep increases the risk of serious problems, including cardiovascular disease. Now Massachusetts General Hospital (MGH) investigators have discovered one way that sleep protects against the buildup of arterial plaques called atherosclerosis. In their paper published in Nature, the researchers describe the mechanism by which insufficient sleep increases production of inflammatory white blood cells known to be major contributors to atherosclerosis.
“We have discovered that sleep helps to regulate the production in the bone marrow of inflammatory cells and the health of blood vessels and that, conversely, sleep disruption breaks down control of inflammatory cell production, leading to more inflammation and more heart disease,” says Filip Swirski, senior author of the paper.
“We also have identified how a hormone in the brain known to control wakefulness controls processes in the bone marrow and protects against cardiovascular disease.”
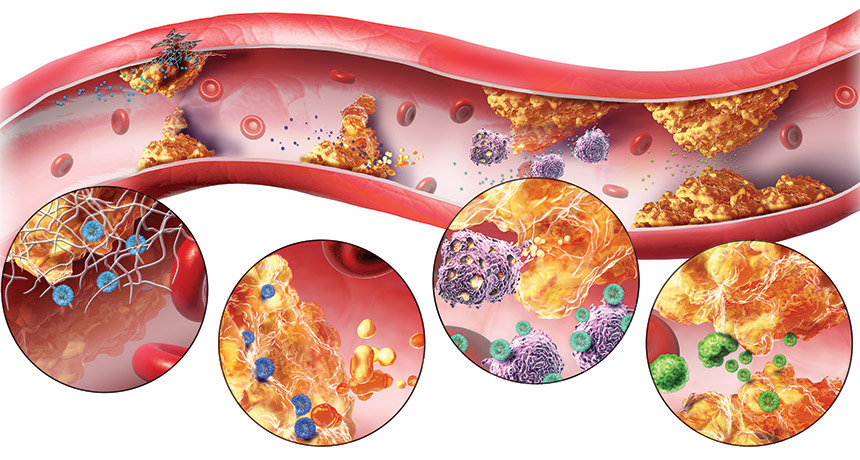
To investigate how insufficient sleep increases atherosclerosis, Swirski’s team subjected mice genetically programmed to develop atheroslcerosis to repeated interruptions of their sleep, similar to the experience of someone constantly waking up because of noise or discomfort. While there were no changes in weight, cholesterol levels or glucose tolerance in the sleep-deprived mice, they developed larger arterial plaques and had higher levels of monocytes and neutrophils — inflammatory cells that contribute to atherosclerosis — in their blood vessels.
Further experiments revealed that the sleep-deprived mice had a nearly two-fold increase in the production of stem cells in their bone marrow that give rise to white blood cells. A hormone called hypocretin, produced in the brain structure called the hypothalamus and known to have a role in the regulation of sleep, was found to play an unexpected role in controlling white blood cell production. While normally produced at high levels when animals — including humans — are awake, hypocretin levels were significantly reduced in the sleep-deprived mice.
The researchers found that hypocretin regulates production of white blood cells through interaction with neutrophil progenitors in the bone marrow. Neutrophils, they discovered, induce monocyte production through release of a factor called CSF-1, and experiments with mice revealed that hypocretin controls CSF-1 expression, monocyte production and the development of arterial plaques.
In sleep-deprived animals, the drop in hypocretin led to increased CSF-1 production by neutrophils, elevated monocyte production and accelerated atherosclerosis.
“This is a direct demonstration that hypocretin is also an important inflammatory mediator,” says Swirski, an associate professor of Radiology at Harvard Medical School. “We now need to study this pathway in humans, explore additional mechanisms by which proper sleep maintains vascular health and further explore this newly identified neuro-immune axis.”
Source: McAlpine CS, Kiss MG, Rattik S, He S, Vassalli A, Valet C, Anzai A, Chan CT, Mindur JE, Kahles F, Poller WC, Frodermann V, Fenn AM, Gregory AF, Halle L, Iwamoto Y, Hoyer FF, Binder CJ, Libby P, Tafti M, Scammell TE, Nahrendorf M, Swirski FK. Sleep modulates haematopoiesis and protects against atherosclerosis. Nature, 2019 DOI: 10.1038/s41586-019-0948-2











