by Jim English and John Steinke, L.Ac
For the past sixty years, doctors have prescribed hormones to help women cope with menopausal symptoms and prevent age-related disorders such as heart disease and osteoporosis. This routine practice came to an abrupt halt in 2002 after the National Institutes of Health (NIH) cancelled one of the largest clinical trials ever conducted on hormone replacement therapy (HRT).
The truncated study, the Women’s Health Initiative (WHI), involved 16,608 women between the ages of 50 and 79 who randomly took either a placebo or a pill containing estrogen and progestin everyday. The lead investigators expected to prove that the hormone combo would be shown to reduce bone fractures and heart disease.
Five years into the planned eight year trial the researchers were shocked to learn that women receiving the hormone therapy had 29 percent more heart attacks, 41 percent more strokes, a 26 percent increase in invasive breast cancer and more than twice as many blood clots compared to those taking placebos.
Lead researcher Marcia Stefanick observed that the study provided, “…very definitive information about how big the risks are and how small the benefits are. With 6 million women on estrogen plus progestin in the country, we really needed to get that message out there in such a way that the medical community would recognize that this is not just a little controversy anymore.”
Sharp Decline in Breast Cancer Rates
One year after the NIH study was stopped, worries about hormone therapy were reignited after U.S. government figures for 2003 revealed an unexpected 7 percent drop in new cases of breast cancer in women aged 50 or older. By contrast, in the 1990s, incidence of breast cancer in older women rose by about 0.5 percent per year.
While some health authorities argued that the decline was temporary and predicted that breast cancer rates would rise again, a paper in the April 19, 2007 issue of the New England Journal of Medicine contained even more bad news for HRT backers. According to the NEJM article, breast cancer rates dropped a stunning 9 percent between 2001 and 2004. The trend was even stronger in cancers fueled by estrogen (i.e., estrogen-receptor positive). Rates for those forms of breast cancer fell by almost 15 percent among women ages 50 to 69, the group most likely to have been on hormone pills.
The NEJM study has confirmed what many health experts originally suspected – that recent drops in breast cancer rates are not a statistical fluke, but a very real result of women abandoning hormone replacement therapy.
HRT Linked to Increased Incidence of Ovarian Cancer
On April 18, 2007, one day prior to the release of the NEJM paper, the British medical journal The Lancet released a study that showed that women taking HRT for more than five years were 20 percent more likely to develop, and die from, ovarian cancer than women who never took hormones. Titled the Million Women Study, the research covered 1.3 million British women from 1996 to 2001.
While the Lancet paper revealed a clear link between HRT and ovarian cancer, HRT supporters once again rushed to the defense, pointing out that, in absolute terms, the risks were very small, resulting in only one extra case of ovarian cancer in every 2,500 women and only one extra death in every 3,300 women. When one considers that at least six million American women were taking HRT prior to this study (some estimates put the total number for all forms of HRT closer to 15 million), the numbers extrapolate to a sobering 2,000 additional deaths from ovarian cancer in the United States each and every year.
One piece of goods news contained in the Lancet article was that once women stop taking HRT the increased risks for ovarian cancer disappeared quickly.
In the wake of all the negative reports the number of prescriptions for hormone therapy dropped by 67 percent between 2001 (61 million prescriptions) and 2004 (21 million prescriptions). Much of the decline occurred as physicians adopted a more prudent approache to treatment. Whereas some doctors simply stopped writing prescriptions for patients over concerns for the long-term risks, others continued to prescribe hormone therapy, but only for severe menopausal symptoms, and then at the lowest doses and shortest time periods possible.
Additionally, millions of women voluntarily chose to abandon hormone therapy on their own, preferring to seek safer and more effective alternatives to synthetic hormones to relieve hot flashes, weight gain and fatigue. Fortunately, viable options do exist.
Viable Alternatives to HRT
Alternative physicians have warned women of the dangers of synthetic hormone therapy for decades, most notably the late John R. Lee, MD, author of the best selling books What Your Doctor May Not Tell You About Perimenopause and What Your Doctor May Not Tell You About Menopause. Dr. Lee and other leading alternative physicians have long advised that women switch from HRT to a form of estrogen that is biologically identical to that produced by the body.
In the United States several compounding pharmacies provide both bi-est and tri-est estrogen preparations specifically for this purpose. Additionally, many women have benefited by switching to a natural form of progesterone, such as that described by Dr. Lee, in place of the synthetic progesterone implicated in the WHI study (medroxyprogesterone acetate).
Natural Options
Western medicine has relied on the use of synthetic hormones and pharmaceutical agents for over 60 years. By contrast, for thousands of years women throughout the world have traditionally turned to plants and tonic herbs to support health and provide support for a wide range of ailments. Rather than exerting the harsh, overt and direct actions of hormones and prescription medications, tonic herbs gently rebalance the body to restore health without harmful side effects.
In China millions of women rely on modern tonic herbal formulas to provide support for issues facing women during and after menopause:
- Discomfort that arises as the ovaries lose function
- Increased risk of heart disease as estrogen production declines
- Loss of bone density that often accelerates after cessation of menstrual periods
To understand why herbs are so effective we need to briefly review the processes involved in the transition period moving through perimenopause into menopause.
Reproductive Cycles
An adult woman’s reproductive life occurs in three distinct phases. First are the childbearing years, characterized by cyclic ovulation and menstruation. In the second phase, called perimenopause, women still have menstrual periods, but the first signs of menopause and irregular ovulation have begun to appear. Many women notice these first signs of perimenopause in their mid-40s, but symptoms can appear in some women as early as their mid-30s.
Perimenopause is marked as the time when periods first become irregular up until one year after the final period, a phase covering anywhere from two to eight years. At this point a woman enters the third phase, known as menopause or the climacteric, characterized by the cessation of ovulation and menstruation. These three phases each have distinct patterns of hormone balance and endocrine gland activity as well as distinct physical, mental and emotional patterns.
Understanding Perimenopause
Every year approximately 2 million American women enter perimenopause. While many experience relatively minor symptoms, about 30 percent have moderate to severe symptoms that can last up to ten years. Beginning between the ages of 35 and 55, perimenopause starts when the ovaries begin to lose their ability to produce estrogen and progesterone. The resulting drop in hormonal levels upsets the normal delicate hormonal balance and interplay between the hypothalamus, the pituitary gland and the ovaries, causing symptoms such as sleep difficulty, decreased libido, and intense irritability and mood fluctuations in women who’ve never experienced moodiness before.
To adapt to fluctuating estrogen and progesterone levels, the body struggles to restore estrogen production by increasing production of two hormones that stimulate estrogen production; Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH). Additionally, the adrenal glands and fat cells begin to secrete estrogen, but eventually estrogen levels are depleted.
The result of this process is the onset of symptoms that can include irregular cycles, missed periods, hot flashes, night sweats, palpitations, emotional fragility and depression, headaches, memory loss, insomnia, loss of libido, vaginal dryness and dry skin. Additionally, the changes in hormonal balance are known to contribute to several age-related disorders in women, including atherosclerosis, heart disease and stroke and loss of bone mass (osteoporosis).
Traditional Herbs for Peri- and Menopausal Symptoms
According to Subhuti Dharmananda in The Endocrine Effect of Chinese Medicine, “Chinese herbs act by stimulating the production of hormones, altering the condition of hormone receptors or changing the rate of catabolism of hormones, rather than by providing the hormones or hormone analogs that function the same as hormones.”
In the case of one advanced Chinese herbal formula, animal studies have shown that the formula is capable of markedly increasing the estrogen receptor levels in the pituitary, hypothalamus and ovaries in aged subjects.
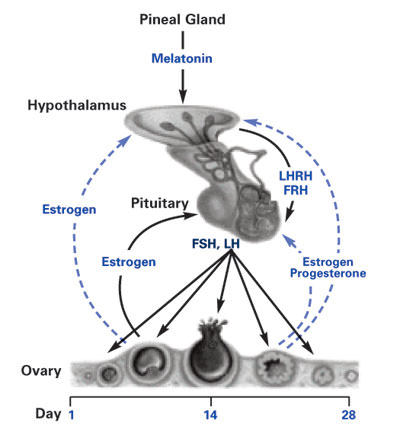
Fig. 1. Female reproductive homeostat from The Neuroendocrine Theory of Aging,
by Ward Dean, MD., illustration by Jim English.
Help for Hot Flashes
The formula, designed by famed master herbalist, Dr. Dexin Yan, was shown to support the autonomic nervous system, the body’s “thermostat” responsible for controlling automatic physiological functions (cardiovascular, digestive and respiratory functions) and responses (contraction and dilation of blood vessels, perspiration and urination).
Hot flashes are one the most common symptoms of perimenopause, and occur when brain neurotransmitters become imbalanced as a result of fluctuating levels of estrogen. In a major study conducted by the Shanghai Center for Modern Traditional Chinese Medicine, fifty women, aged 44 to 60 years, were treated with Dr. Yan’s formula for menopausal symptoms that included hot flashes, anxiety, emotional instability, headaches, dizziness, restlessness, spontaneous sweating, aching of the legs and low back, uncontrollable crying and depression.
After taking Dr. Yan’s formula (shortest administration period, 1 month; longest, 3 months), 30 patients reported complete relief of all symptoms, 13 experienced marked improvement, and three reported some improvement.
The ability of Dr. Yan’s formula to reduce hot flashes and other autonomic symptoms (i.e., sweating, headaches) indicate that the formula has a positive impact on neurotransmitter function that can restore balance to the hypothalamic, pituitary, ovarian homeostat (Fig. 1).
Improving Blood Circulation
Dr. Yan’s formula has been shown to improve circulation to the heart and brain by promoting vessel dilation and inhibiting the clumping of red blood cells. Numerous animal studies support this finding and indicate that the formula improves microcirculation in the capillaries, inhibits formation of thromboxane A2 to prevent blood clots, and reverses platelet aggregation to improve blood flow.
The benefits of improved blood flow, including improved vessel dilation and reduced blood viscosity, also aid in preserving the function of the organs and glands that determine healthy endocrine function as women age.
Osteoporosis Support
By supporting improved blood flow, Dr. Yan’s formula can also help in preventing bone loss as women enter postmenopause. After menopause, bone loss accelerates for 3-5 years, at a rate of 1.5 to 5 percent per year. Bone loss then continues at a lower level of around 1 to 1.5 percent loss per year on average.
Six of the herbs contained in Dr. Yan’s formula are used in China in the treatment and reversal of Avascular Necrosis of The Femoral Head (AVN). In this severe disorder, the head of the femur at the hip collapses from a lack of blood flow that leads to the destruction of bone tissue. This condition is commonly caused by chronic use of corticosteroid therapy.
The herbs contained in Dr. Yan’s formula play a central role in the restoration of blood flow and bone mass density in this condition. Two herbs in particular – Angelica sinensis and cordyceps – are vital to reversing this disorder and form the foundation of the formula. Just as the formula aids in diminishing the symptoms of menopausal syndrome, it should also provide women with protection against osteoporosis.
Dr. Yan’s Formula for Daily Use
Dr. Yan’s formula, available in the U.S. as FemmePhase®, is an all-natural herbal blend designed to be taken at the earliest sign of symptoms to ease the transition through perimenopause and menopause. After menopause, continued daily supplementation can aid in maintaining endocrine, circulatory and skeletal performance to ameliorate age-related health issues and optimize overall health.